Vaginal cancer is a rare but serious condition that affects the muscular tube that connects your uterus with your outer genitals. It can cause symptoms such as abnormal bleeding, discharge, pain, and urinary problems. It can also spread to other parts of your body if not treated early.
In this blog post, we will cover everything you need to know about vaginal cancer, including its types, causes, risk factors, diagnosis, treatment options, and future directions. We hope this information will help you understand this disease better and take action if needed.
Vaginal Cancer: Introduction
Vaginal cancer is a type of cancer that starts in the cells that line the surface of your vagina. The vagina is also called the birth canal because it is where a baby passes through during delivery. The vulva, or the external female genitalia, is where the vagina opens after beginning at the cervix, the bottom portion of the uterus.
There are different types of vaginal cancer, depending on the type of cell where the cancer began. The most common type is squamous cell carcinoma, which accounts for about 85% of all vaginal cancers. It develops in the thin, flat cells that line the inside of the vagina, and is most common in the upper part of the vagina near the cervix.
Other types of vaginal cancer include:
- Adenocarcinoma, which starts in your vagina’s surface glandular cells
- Melanoma, which forms in your vagina’s pigment-producing cells (melanocytes)
- Sarcoma, which forms in the muscle or connective tissue cells in the vaginal walls
It is very rare, affecting only about 1 in every 100,000 women each year. It is more common in older women, especially those over 60 years old.But it can strike anyone, even young children.

What are the symptoms of vaginal cancer?
Early vaginal cancer may not show any symptoms at all. It may manifest as the following signs and symptoms as it progresses:
- uncommon vaginal bleeding, such as after sex or after menopause
- Watery vaginal discharge
- A lump or mass in your vagina
- Painful urination
- Frequent urination
- Constipation
- Pelvic pain
These symptoms are not specific to vaginal cancer and can be caused by other conditions as well. However, if you have any of these symptoms, you should see your doctor as soon as possible for a check-up.
Types of vaginal cancer
While it is relatively uncommon, it manifests in various types, originating from distinct vaginal cell types.
Squamous Cell Carcinoma
Squamous cell carcinomas account for almost 90% of vaginal cancer cases. These cancers emerge from the squamous cells comprising the vaginal epithelial lining. Primarily situated in the upper vaginal region near the cervix, if left untreated, they can progress deeper into and eventually breach the vaginal wall. They also have the potential to metastasize to neighboring tissues and other body parts, particularly the lungs, liver, and bones.
The development of squamous cell vaginal cancers is typically gradual. Initially, certain normal vaginal cells undergo pre-cancerous alterations (VAIN). Subsequently, some of these pre-cancerous cells transform into cancer cells, a process that spans several years.
Adenocarcinoma
Adenocarcinomas arise from gland cells and constitute around 10% of vaginal cancer cases. The prevalent subtype affects women over 50. Another variant, known as clear cell adenocarcinoma, predominantly affects young women exposed to diethylstilbestrol (DES) while in the womb. More details on DES and clear cell carcinoma can be found in the section on Vaginal Cancer Risk Factors.
Less Common Vaginal Cancers
Melanoma
Melanomas initiate in pigment-producing cells responsible for skin color. While these cancers are typically found on sun-exposed skin areas, they can also form within the vagina or other internal organs. Melanomas account for less than 3% of vaginal cancer cases.
Typically affecting the lower or outer vaginal region, melanoma tumors vary in size, color, and growth pattern. Further information can be accessed in the Melanoma Skin Cancer section.
Sarcoma
Sarcomas originate in bone, muscle, or connective tissue cells. Sarcomas constitute fewer than 3% of vaginal cancer cases, forming deep within the vaginal wall rather than its surface.
Various sarcoma types exist. Rhabdomyosarcoma, prevalent in children and rare in adults, is the most common vaginal sarcoma. A sarcoma named leiomyosarcoma is more frequent among adults, primarily affecting women over 50.

What are the causes of vaginal cancer?
The exact cause of vaginal cancer is not known. However, some factors may increase your risk of developing this disease. These include:
- Exposure to diethylstilbestrol (DES), a synthetic form of estrogen that was given to some pregnant women between 1940 and 1971 to prevent miscarriage. Women who were exposed to DES before birth have a higher risk of developing clear cell adenocarcinoma of the vagina or cervix.
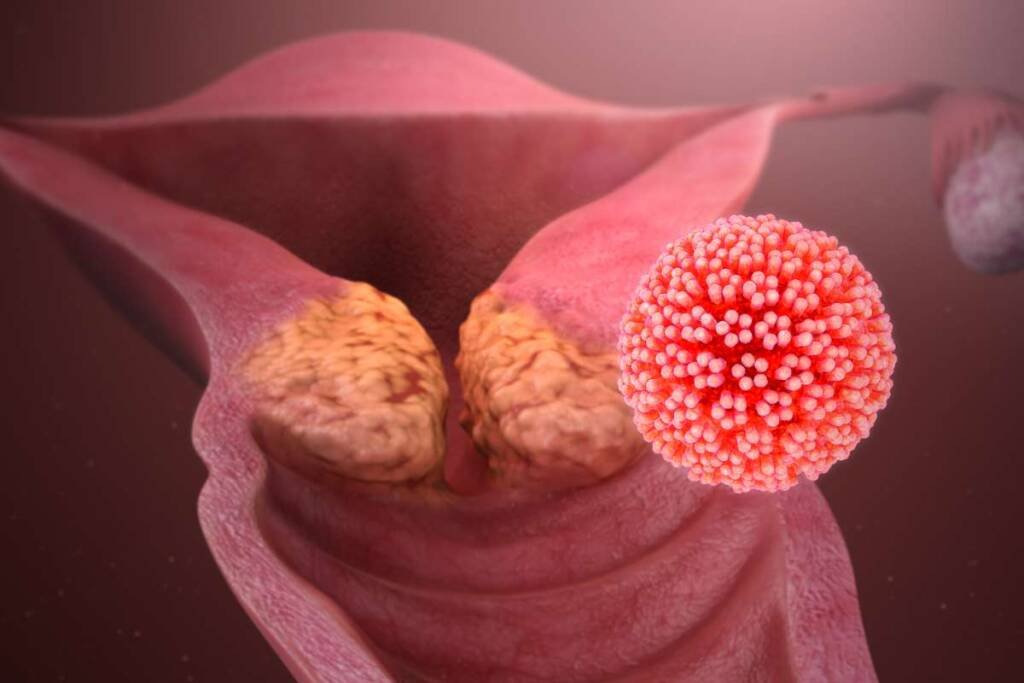
- Human papillomavirus (HPV) infection, a common sexually transmitted infection that can cause genital warts and cervical cancer. Some types of HPV can also cause vaginal cancer, especially squamous cell carcinoma.
- Smoking, which can damage the DNA of your cells and make them more likely to become cancerous.
- Having a history of abnormal Pap tests or cervical cancer, which may indicate that you have precancerous changes in your vagina or cervix that could progress to cancer.
- Having a weakened immune system due to HIV/AIDS or other conditions that make you more vulnerable to infections and cancers.
Related: Endometrial Cancer: Symptoms, Risks, And Treatments
What are the vaginal cancer risk factors?
The following are some elements that could raise your risk of getting vaginal cancer:
- Increasing age. As you become older, your chance of vaginal cancer rises. Most people who are diagnosed with vaginal cancer are older than 60.
- Being female. Vaginal cancer only affects women.
- Having multiple sexual partners. Having sex with many different people increases your exposure to HPV and other sexually transmitted infections that can cause vaginal cancer.
- Having sex at an early age. Having sex before age 18 increases your exposure to HPV and other sexually transmitted infections that can cause vaginal cancer.
- Not getting vaccinated against HPV. The HPV vaccine can protect you from some types of HPV that can cause cervical and vaginal cancers. The vaccine is recommended for girls and boys between ages 9 and 26.
Stages of vaginal cancer
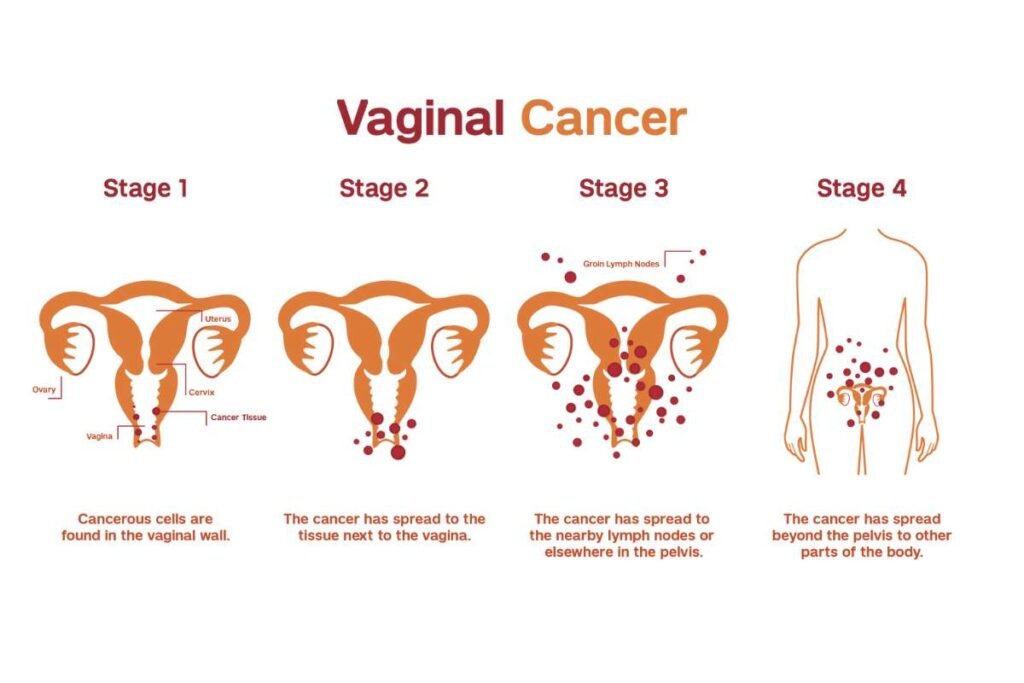
Once a diagnosis of vaginal cancer is made, further examinations are conducted to determine if the cancerous cells have extended within the vaginal area or metastasized to other body regions. Cancer can disseminate through three main methods. It can spread from its initial site to different body parts. Vaginal intraepithelial neoplasia (VaIN) involves the identification of abnormal cells in the vaginal lining. The stages of vaginal cancer are categorised as follows: Stage I, Stage II, Stage III, and Stage IV. It’s important to note that vaginal cancer has the potential to reoccur even after undergoing treatment.
How is vaginal cancer diagnosed?
Sometimes vaginal cancer is discovered during a normal pelvic exam before symptoms and indications show up. Your doctor will carefully examine your outer genitalia during the pelvic exam, put two fingers of one hand into your vagina, and push the other hand on your abdomen to feel your uterus and ovaries. Additionally, he or she places a speculum inside of your vagina. Your doctor can examine your vagina and cervix for anomalies using the speculum, which opens your vaginal canal.
A Pap test could also be performed by your doctor. Pap tests are typically used to screen for cervical cancer, but they can occasionally pick up vaginal cancer cells as well. A Pap test involves scraping some cells from your cervix and vagina and sending them to a laboratory for analysis.
Based on the results of the pelvic exam and Pap test, your doctor may conduct other tests to confirm the diagnosis of vaginal cancer, such as:
- Colposcopy, which is an examination of your vagina with a special lighted magnifying instrument called a colposcope. Colposcopy allows your doctor to magnify the surface of your vagina to see any areas of abnormal cells.
- Biopsy, which is a procedure to remove a sample of suspicious tissue to test for cancer cells. Your doctor may take a biopsy of tissue during a colposcopy exam or with a needle or scalpel.
- Imaging tests, such as X-rays, CT scans, MRI scans, or PET scans, which can show whether cancer has spread to other parts of your body.
- Endoscopy, which is a procedure that uses tiny cameras to see inside your body. Endoscopy can help your doctor see inside your bladder (cystoscopy) and your rectum (proctoscopy) to check for cancer spread.

What are the vaginal cancer treatment options?
Treatment for vaginal cancer depends on several factors, such as the type and stage of the cancer, your overall health, and your preferences. The main treatment options for vaginal cancer include:
Surgery
Surgery involves removing the tumour along with some nearby healthy tissue. Surgery may be used to treat early-stage vaginal cancer or to relieve symptoms in advanced-stage vaginal cancer. The following surgical procedures could be used to treat vaginal cancer:
- Removal of small tumors or lesions.In order to ensure that all cancer cells have been eliminated, cancer that is localised to the surface of your vagina may be taken away along with a thin margin of surrounding healthy tissue.
- Laser surgery. Laser surgery uses a high-intensity beam of light to vaporise cancer cells on the surface of your vagina.
- Wide local excision. Wide local excision is a procedure that removes the tumor and some surrounding healthy tissue from your vagina.
- Vaginectomy. Vaginectomy is a procedure that removes part or all of your vagina. Depending on how much tissue is removed, you may need reconstructive surgery to rebuild your vagina using skin grafts or flaps from other parts of your body.
- Radical hysterectomy. Radical hysterectomy is a procedure that removes your uterus, cervix, ovaries, fallopian tubes, and nearby lymph nodes. This surgery is usually done if the cancer has spread beyond your vagina.
- Pelvic exenteration. Pelvic exenteration is a major surgery that removes all of the organs in your pelvic area, including your bladder, rectum, vagina, uterus, cervix, ovaries, and fallopian tubes. You will need reconstructive surgery to create new ways for urine and stool to leave your body.
Radiation therapy
Radiation therapy uses high-energy beams, such as X-rays or protons, to kill cancer cells or stop them from growing. Radiation therapy may be used alone or in combination with surgery or chemotherapy to treat vaginal cancer.There are two techniques to provide radiation therapy:
- External beam radiation therapy. External beam radiation therapy delivers radiation from a machine outside your body to the tumor and nearby areas. You may receive external beam radiation therapy five days a week for several weeks.
- Internal radiation therapy (brachytherapy). Internal radiation therapy involves placing radioactive material inside your vagina or uterus for a short time. The radioactive material delivers a high dose of radiation directly to the tumor while sparing nearby healthy tissues.
Chemotherapy
Chemotherapy employs medications to either kill or stop the growth of cancer cells. Chemotherapy may be given by mouth, injection, or infusion into a vein. Chemotherapy may be used alone or in combination with surgery or radiation therapy to treat vaginal cancer. Chemotherapy may also be used to shrink tumors before surgery or radiation therapy or to relieve symptoms in advanced-stage vaginal cancer. Cisplatin is an example of a drug that doctors may use to manage vaginal cancer.
What are the emerging vaginal cancer treatment options?
Researchers are studying new ways to treat vaginal cancer more effectively and with fewer side effects. Some of the emerging vaginal cancer treatment options include:
- Immunotherapy, which uses drugs or substances that stimulate the immune system to fight cancer cells. Immunotherapy drugs that are being tested for vaginal cancer include nivolumab (Opdivo), ipilimumab (Yervoy), and durvalumab (Imfinzi).
- Gene therapy, which uses viruses or other methods to deliver genes into cancer cells to make them more sensitive to treatment or to kill them directly. Gene therapy trials for vaginal cancer are using a virus called adenovirus to deliver a gene called p53, which is a tumor suppressor gene that is often mutated in cancer cells.
- Photodynamic therapy, which uses a drug that makes cancer cells more sensitive to light and then exposes them to a special type of light that kills them. Photodynamic therapy may be used to treat precancerous lesions or early-stage vaginal cancer.
- Nanomedicine, which uses tiny particles or devices that can deliver drugs or radiation directly to the tumor site or target specific molecules on the cancer cells. Nanomedicine may help reduce the side effects of chemotherapy or radiation therapy and increase their effectiveness.
Future directions of vaginal cancer
The future of vaginal cancer research and treatment is promising. Scientists are working on developing better ways to prevent, detect, diagnose, treat, and cure vaginal cancer. Some of the future directions of vaginal cancer include:
- Developing new screening methods and tests that can detect vaginal cancer at an earlier stage and more accurately
- Identifying new biomarkers and genetic mutations that can predict the risk, prognosis, and response to treatment of vaginal cancer
- Finding new ways to prevent HPV infection and cervical cancer, which can reduce the risk
- Improving the quality of life and survival of vaginal cancer survivors by addressing their physical, emotional, social, and sexual needs
- Increasing awareness and education about vaginal cancer among women, health care providers, and the general public
Related: Urethral Cancer: A Rare but Serious Urological Condition
Conclusion
Vaginal cancer is a rare but serious condition that affects the muscular tube that connects your uterus with your outer genitals. It can cause symptoms such as abnormal bleeding, discharge, pain, and urinary problems. It can also spread to other parts of your body if not treated early.
It can be treated with surgery, radiation therapy, chemotherapy, or targeted therapy, depending on the type and stage of the cancer, your overall health, and your preferences. There are also new and emerging treatment options that are being tested in clinical trials.
The best way to prevent vaginal cancer is to avoid exposure to risk factors such as DES, HPV infection, smoking, and abnormal Pap tests. You should also get vaccinated against HPV if you are eligible and have regular pelvic exams and Pap tests as recommended by your doctor.
FAQ’s
How common is vaginal cancer?
Vaginal cancer is very rare, affecting only about 1 in every 100,000 women each year. It accounts for less than 1% of all gynecologic cancers.
How is vaginal cancer staged?
Vaginal cancer is staged according to the size and extent of the tumor and whether it has spread to nearby lymph nodes or distant organs. The stages range from stage 0 (carcinoma in situ) to stage IV (metastatic disease).
Can vaginal cancer be cured?
Vaginal cancer can be cured if it is found and treated at an early stage. The five-year survival rate for stage I vaginal cancer is about 84%. However, the survival rate drops significantly as the stage increases. The five-year survival rate for stage IV vaginal cancer is about 15%.