The US Food and Drug Administration (FDA) has initiated a priority review of exagamglogene autotemcel (exa-cel), a therapy developed by Vertex Pharmaceuticals and CRISPR Therapeutics for sickle cell disease (SCD). The FDA is expected to make a decision regarding approval by December 8th.
In addition to the priority review, the FDA is conducting a standard review of the CRISPR-based therapy for transfusion-dependent thalassemia (TDT), with a verdict expected by March 30th of next year.
This update coincides with the release of new findings from two pivotal trials (CLIMB-111 and CLIMB-121) and a longer-term observational study (CLIMB-131) conducted by Vertex and CRISPR. The results demonstrate that exa-cel continues to meet primary and secondary endpoints in a group of 83 patients with TDT or SCD over a follow-up period of up to 43.7 months.
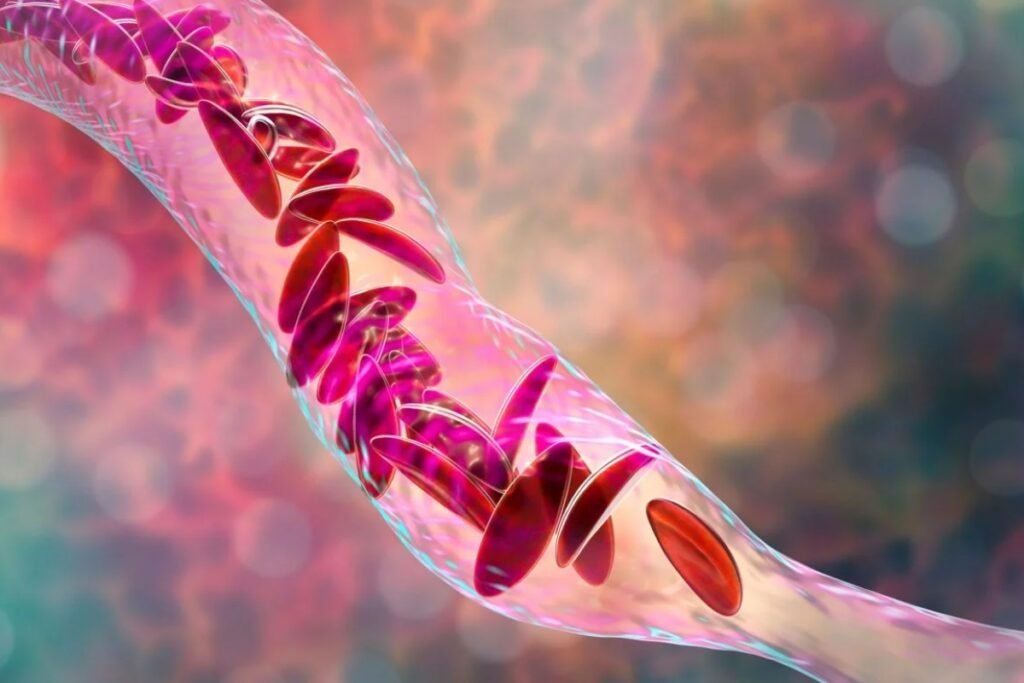
Exa-cel employs an ‘ex vivo’ application of CRISPR gene-editing, modifying the patient’s own cells outside the body to produce fetal hemoglobin (HbF). This substitute for regular hemoglobin proves beneficial for individuals with SCD and beta thalassemia by replacing the malformed and defective hemoglobin, thereby preventing painful vaso-occlusive crises (VOCs) in SCD and eliminating the need for blood transfusions in TDT patients.
Among the evaluated subjects with TDT, 24 out of 27 (89%) had not required a transfusion for at least six months, meeting the primary endpoint. Of the remaining three patients, two experienced a decrease in transfusion volumes, and one has remained transfusion-free for nearly three months.
In the SCD group, 16 out of 17 evaluable patients (94%) have been free from VOCs for a minimum of 12 months following the one-time treatment. The average duration of VOC-free status was over 18 months, with the longest period reaching three years.
The updated results will be presented at the upcoming European Hematology Association (EHA) congress.
If approved, exa-cel could potentially benefit approximately 32,000 eligible patients in the United States. However, Vertex has yet to disclose pricing plans or sales projections for the therapy.
The companies have also submitted applications for approval of exa-cel in the European Union and the United Kingdom, with decisions expected in the latter part of this year.
Vertex’s CEO, Reshma Kewalramani, stated, “Exa-cel holds the promise to be the first CRISPR gene-editing therapy to be approved, and we continue to work with urgency to bring this treatment with transformative potential to patients who are waiting.”
Vertex and CRISPR’s timeline keeps them ahead of bluebird bio, their closest competitor with the gene-editing therapy lovotibeglogene autotemcel (lovo-cel) for SCD, which has experienced delays.
While bluebird bio has gained approval for its TDT therapy betibeglogene autotemcel (beti-cel), marketed as Zynteglo, from the FDA, it has chosen not to commercialize it in Europe, citing reimbursement policies that render high-priced, one-time therapies unviable.