Hematological malignancies are cancers that affect the blood, bone marrow, and lymph nodes. They include leukemia, lymphoma, and multiple myeloma. These diseases are often difficult to treat and have poor prognosis. However, in recent years, a new treatment option has emerged that offers hope and cure for some patients who have no other options. This treatment is called CAR T-cell therapy.
CAR T-cell therapy is a type of immunotherapy that uses genetically modified immune cells to fight cancer in a personalized and targeted way. It sounds amazing, right? But before getting too excited, one should know that CAR T-cell therapy is not a magic bullet. It has its pros and cons, and it may not be suitable or available for everyone. In this blog, we will explain what CAR T-cell therapy is, how it works, what are its benefits and risks, and how it compares to other treatments for hematological malignancies.
What is CAR T-Cell Therapy?
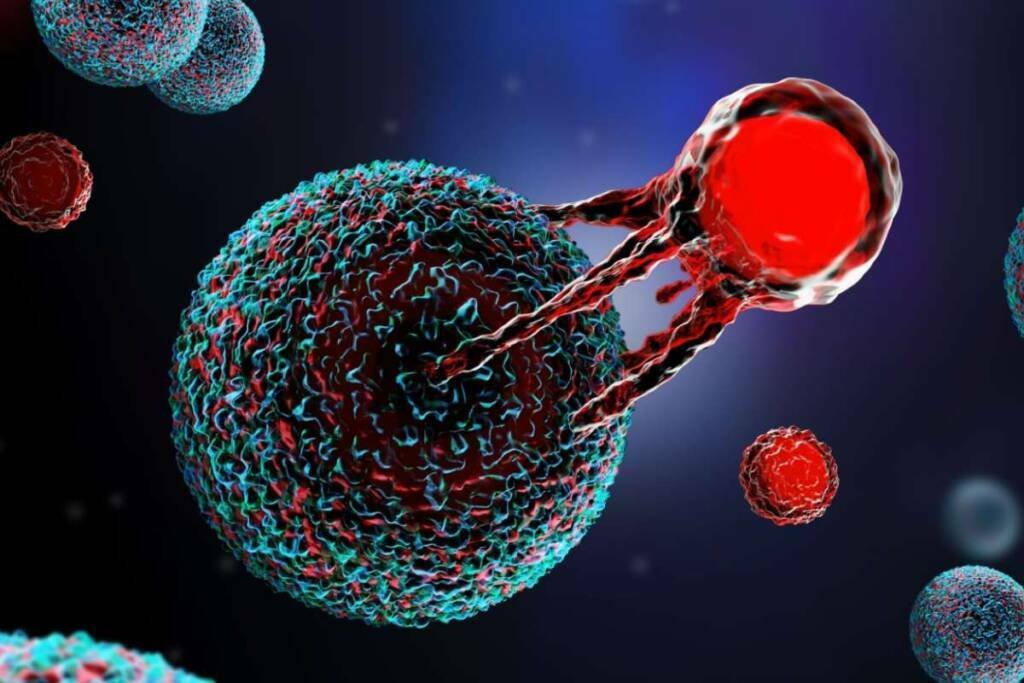
CAR T-cell therapy is a treatment that uses the patient’s own immune cells to attack cancer cells. The immune cells that are used are called T cells, which are white blood cells that play a key role in the immune system. They can recognize and destroy foreign invaders, such as bacteria, viruses, and cancer cells. However, sometimes cancer cells can evade or suppress the immune system, making it harder for T cells to find and kill them.
That’s where CAR T-cell therapy comes in. CAR stands for chimeric antigen receptor, which is a synthetic molecule that can bind to a specific protein (antigen) on the surface of cancer cells. By engineering T cells to express CARs, scientists can make them more effective at targeting and eliminating cancer cells.
The process of CAR T-cell therapy involves several steps:
- First, T cells are collected from the patient’s blood through a procedure called leukapheresis.
- Second, the T cells are sent to a laboratory where they are genetically modified to express CARs using a viral vector.
- Third, the modified T cells are multiplied in the laboratory until they reach a sufficient number.
- Fourth, the modified T cells are infused back into the patient’s bloodstream where they can seek out and destroy cancer cells.
How Does CAR T-Cell Therapy Work?
The main advantage of CAR T-cell therapy is that it can target cancer cells in a specific and personalized way. Unlike chemotherapy or radiation therapy, which can affect both healthy and cancerous cells, CAR T-cell therapy only targets cells that express the antigen that matches the CAR. This reduces the risk of harming normal tissues and organs.
Another advantage of CAR T-cell therapy is that it can create a long-lasting immune response. The modified T cells can persist in the body for months or even years after the infusion, providing continuous surveillance and protection against cancer recurrence. Some patients may achieve complete remission or cure after a single dose of CAR T-cell therapy.
However, CAR T-cell therapy is not without challenges and limitations. One of the main challenges is finding the right antigen to target. The antigen must be present on most or all cancer cells, but not on normal cells. Otherwise, the CAR T cells may attack healthy tissues and cause severe side effects. For example, CD19 is a common antigen used to target B-cell malignancies, such as leukemia and lymphoma. However, CD19 is also expressed on normal B cells, which are important for producing antibodies and fighting infections. Therefore, patients who receive CD19-targeted CAR T-cell therapy may experience B-cell depletion and immunodeficiency.
Another challenge of CAR T-cell therapy is managing its potential toxicities. The most common and serious side effects of CAR T-cell therapy are cytokine release syndrome (CRS) and neurotoxicity. CRS occurs when the activated CAR T cells release large amounts of inflammatory molecules (cytokines) into the bloodstream, causing fever, chills, low blood pressure, organ failure, and even death. Neurotoxicity occurs when the cytokines affect the brain and nervous system, causing confusion, seizures, coma and even death. These side effects can occur within hours or days after the infusion and require intensive monitoring and treatment in specialized centers.
Approved CAR T-Cell Therapies
CAR T-cell therapy is currently approved by the FDA for certain types of hematological malignancies that have relapsed or refractory after two or more lines of standard treatments. Since 2017, the FDA has given approval to six CAR-T cell therapies for blood cancers. The first two CAR-T products to get approved were Kymriah (tisagenlecleucel) and Yescarta (axicabtagene ciloleucel). They are used to treat patients who are 25 years old or younger with B-cell precursor ALL that does not respond or comes back after treatment, and adult patients with DLBCL that relapses or is resistant after two or more types of systemic therapies.
| Table: 1 Approved CAR T-cell Therapies in Hematological malignancies and their cost | ||||
| CAR T-cell therapy | Year of approval | Approved indication | Cost | |
| Kymriah (Tisagenlecleucel) | 2017 | Patients up to 25 years of age with B-cell precursor acute lymphoblastic leukemia (ALL) that is refractory or in second or later relapse | $475,000 for ALL; $373,000 for DLBCL | |
| 2018 | Adult patients with relapsed or refractory large B-cell lymphoma after two or more lines of systemic therapy, including diffuse large B-cell lymphoma (DLBCL) not otherwise specified, high grade B-cell lymphoma and DLBCL arising from follicular lymphoma. | |||
| 2022 | Adult patients with relapsed or refractory FL after two or more lines of systemic therapy. This indication is approved under accelerated approval based on response rate and duration of response. Continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trials. | |||
| Yescarta (Axicabtagene ciloleucel) | 2017 | Adult patients with relapsed or refractory large B-cell lymphoma after two or more lines of systemic therapy, including DLBCL not otherwise specified, primary mediastinal large B-cell lymphoma, high grade B-cell lymphoma, and DLBCL arising from follicular lymphoma. | $373,000 | |
| 2021 | Adult patients with relapsed or refractory FL after two or more lines of systemic therapy. This indication is approved under accelerated approval based on response rate. Continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trials | |||
| 2022 | Adult patients with large B-cell lymphoma that is refractory to first-line chemoimmunotherapy or that relapses within 12 months of first-line chemoimmunotherapy | |||
| Tecartus (Brexucabtagene autoleucel) | 2020 | Relapsed or refractory mantle cell lymphoma in adults | $373,000 | |
| 2021 | Adult patients with relapsed or refractory B-cell precursor acute lymphoblastic leukemia | |||
| Breyanzi (Lisocabtagene maraleucel) | 2021 | Relapsed or refractory large B-cell lymphoma in adults after two or more lines of systemic therapy, including DLBCL, high-grade B-cell lymphoma, primary mediastinal large B-cell lymphoma, and follicular lymphoma grade 3B | $410,300 | |
| 2022 | Relapsed or refractory large B-cell lymphoma in adults after two or more lines of systemic therapy, including DLBCL, high-grade B-cell lymphoma, primary mediastinal large B-cell lymphoma, and follicular lymphoma grade 3B Refractory disease to first-line chemoimmunotherapy or relapse within 12 months of first-line chemoimmunotherapy; Refractory disease to first-line chemoimmunotherapy or relapse after first-line chemoimmunotherapy and are not eligible for hematopoietic stem cell transplant (HSCT) due to comorbidities or age. | |||
| Abecma (Idecabtagene vicleucel) | 2021 | Relapsed or refractory multiple myeloma in adults after four or more prior lines of therapy, including an immunomodulatory agent, a proteasome inhibitor, and an anti-CD38 monoclonal antibody | $419,500 | |
| Carvykti (Ciltacabtagene autoleucel) | 2022 | Relapsed or refractory multiple myeloma in adults after four or more prior lines of therapy, including an immunomodulatory agent, a proteasome inhibitor, and an anti-CD38 monoclonal antibody | $465,000 | |
All of these CAR T-cell therapies target a specific protein on the surface of cancer cells and use the patient’s own T cells that are genetically modified to express a chimeric antigen receptor (CAR). However, they differ in the type of protein they target and the design of the CAR. Here is a brief summary of each therapy and the clinical data that supported its approval:
Kymriah targets CD19, a protein that is expressed on most B-cell malignancies. It uses a CAR that consists of a single-chain variable fragment (scFv) derived from a mouse antibody that recognizes CD19, linked to a CD3-zeta signaling domain and a 4-1BB costimulatory domain. The FDA approval was based on the results of two clinical trials: ELIANA for ALL and JULIET for DLBCL. In ELIANA, 81% of patients achieved overall remission within 3 months of infusion, and the median duration of remission was not reached at a median follow-up of 13.1 months. In JULIET, 52% of patients achieved overall response within 3 months of infusion, and the median duration of response was not reached at a median follow-up of 19.3 months.
Yescarta also targets CD19, but it uses a different CAR that consists of a scFv derived from a murine antibody that recognizes CD19, linked to a CD3-zeta signaling domain and a CD28 costimulatory domain. The FDA approval was based on the results of the ZUMA-1 clinical trial for large B-cell lymphoma. In ZUMA-1, 82% of patients achieved overall response within 1 month of infusion, and the median duration of response was 11.1 months at a median follow-up of 27.1 months. On the basis of ZUMA-7 Yescarta was approved in large B-cell lymphoma that is refractory to first-line chemoimmunotherapy or that relapses within 12 months of first-line Chemoimmunotherapy. The ZUMA-7 study showed that Yescarta significantly improved the event-free survival (EFS) of patients compared to standard therapy. EFS was defined as the time from randomization to the earliest date of disease progression, commencement of new lymphoma therapy, or death from any cause. The median EFS was 8.3 months for patients who received Yescarta and 2.0 months for patients who received standard therapy. The estimated 18-month EFS rate was 41.5% for Yescarta and 17.0% for standard therapy.
Tecartus also targets CD19, but it uses a different CAR that consists of a scFv derived from a fully human antibody that recognizes CD19, linked to a CD3-zeta signaling domain and a CD28 costimulatory domain. The FDA approval in mantle cell lymphoma was based on the results of the ZUMA-2 clinical trial for mantle cell lymphoma. In ZUMA-2, 87% of patients achieved overall response within 1 month of infusion, and the median duration of response was not reached at a median follow-up of 12.3 months. Tecartus was approved based on ZUMA-3.in ALL. Of the 54 patients evaluated for efficacy, 28 achieved complete response within 3 months. With a median follow-up for responders of 7.1 months, the median duration of complete response was not reached; the duration of complete response was estimated to exceed 12 months for more than half the patients.
Breyanzi also targets CD19, but it uses a different CAR that consists of two scFvs derived from fully human antibodies that recognize two distinct epitopes on CD19, linked to a CD3-zeta signaling domain and a 4-1BB costimulatory domain. Breyanzi approval in LBCL who have not responded to, or who have relapsed after, at least two other types of systemic treatment was based on the safety and efficacy in multicenter clinical trials of more than 250 adults with refractory or relapsed large B-cell lymphoma. The complete remission rate after treatment with Breyanzi was 54%. Breyanzi approval in LBCL after one prior therapy was based on the pivotal Phase 3 TRANSFORM trial. A single infusion of Breyanzi significantly outperformed the nearly 30-year standard of care with median event-free survival of 10.1 months vs. 2.3 months and a well-established safety profile.
Abecma targets BCMA, a protein that is expressed on most multiple myeloma cells. It uses a CAR that consists of a scFv derived from a human antibody that recognizes BCMA, linked to a CD3-zeta signaling domain and a 4-1BB costimulatory domain. The FDA approval was based on the results of the KARMMA clinical trial for multiple myeloma. In KARMMA, 72% of patients achieved overall response within 1 month of infusion, and the median duration of response was 11.0 months at a median follow-up of 13.3 months.
Carvykti also targets BCMA, but it uses a different CAR that consists of two scFvs derived from human antibodies that recognize two distinct epitopes on BCMA,linked to a CD3-zeta signaling domain and a CD28 costimulatory domain. The FDA approval was based on the results of the CARTITUDE-1 clinical trial for multiple myeloma. In CARTITUDE-1, 97% of patients achieved overall response within 1 month of infusion, and the median duration of response was not reached at a median follow-up of 12.4 months.
What are the Pros and Cons of Autologous and Allogeneic CAR T-Cell Therapy?
Currently, all the approved CAR T-cell therapies are autologous, meaning that they use the patient’s own T cells. This has several advantages, such as:
- Reducing the risk of graft-versus-host disease (GVHD), which is a potentially fatal complication that occurs when donor cells attack the recipient’s tissues.
- Enhancing the specificity and efficacy of the therapy, as the patient’s T cells are more likely to recognize and kill the patient’s cancer cells.
- Avoiding ethical and regulatory issues related to the use of donor cells.
However, autologous CAR T-cell therapy also has several disadvantages, such as:
- Requiring a long and complex manufacturing process that can take weeks or months, during which the patient’s condition may worsen or change.
- Being dependent on the quality and quantity of the patient’s T cells, which may be impaired or insufficient due to prior treatments or disease progression.
- Being costly and labor-intensive, as each product has to be customized for each patient.
Therefore, there is a growing interest in developing allogeneic CAR T-cell therapy, which uses donor T cells instead of the patient’s own T cells. This has several advantages, such as:
- Reducing the time and cost of manufacturing, as donor T cells can be obtained from healthy volunteers or cord blood banks and processed in large batches.
- Increasing the availability and accessibility of the therapy, as donor T cells can be stored frozen and ready for use whenever needed.
- Improving the quality and potency of the therapy, as donor T cells are not affected by prior treatments or disease status.
However, allogeneic CAR T-cell therapy also has several disadvantages, such as:
- Increasing the risk of GVHD, which can be mitigated by modifying or deleting certain genes in the donor T cells that are responsible for recognizing foreign tissues.
- Increasing the risk of immune rejection, which can be prevented by modifying or deleting certain genes in the donor T cells that are responsible for presenting foreign antigens.
- Raising ethical and regulatory issues related to the use of donor cells.
- Therefore, allogeneic CAR T-cell therapy is still in early stages of development and testing in clinical trials. It remains to be seen whether it can match or surpass the safety and efficacy of autologous CAR T-cell therapy.
Conclusion
CAR T-cell therapy is a revolutionary treatment option for hematological malignancies that can offer hope and cure for some patients who have no other options. However, it is not a panacea for everyone. It has its pros and cons, and it may not be suitable or available for everyone. It also faces several challenges and limitations that need to be overcome by further research and innovation. Therefore, patients who are interested in CAR T-cell therapy should consult their hematologists or oncologists about their eligibility, availability, and affordability of this treatment.
FAQ’s
What is CAR T-cell therapy, and how does it work?
CAR T-cell therapy is a groundbreaking immunotherapy using genetically modified T cells to target cancer. Patient’s T cells are engineered to express chimeric antigen receptors (CARs) that attach to cancer cell antigens. After infusion, CAR T cells locate and destroy cancer cells specifically.
What types of hematological malignancies can CAR T-cell therapy treat?
CAR T-cell therapy is effective against blood cancers like leukemia, lymphoma, and multiple myeloma, utilizing antigens unique to these cancers. It isn’t approved for solid tumors due to antigen specificity.
What are the advantages and disadvantages of CAR T-cell therapy compared to other treatments?
CAR T-cell therapy offers targeted treatment, sparing healthy cells. It can provide long-lasting remission. However, finding the right antigen is critical to prevent harm to healthy cells. Risks include cytokine release syndrome (CRS) and neurotoxicity, requiring careful monitoring.
What are the potential side effects and risks associated with CAR T-cell therapy?
CAR T-cell therapy can lead to severe cytokine release syndrome (CRS) with fever, low blood pressure, and organ failure. Neurotoxicity is possible, causing confusion and seizures. Close monitoring and specialized care are needed to manage these side effects.
Are there different types of CAR T-cell therapies available, and how do they differ?
Yes, approved therapies like Kymriah, Yescarta, Tecartus, Breyanzi, Abecma, and Carvykti target distinct antigens (CD19 or BCMA). They use varying chimeric antigen receptors (CARs) for enhanced effectiveness, based on cancer type and antigen expression.