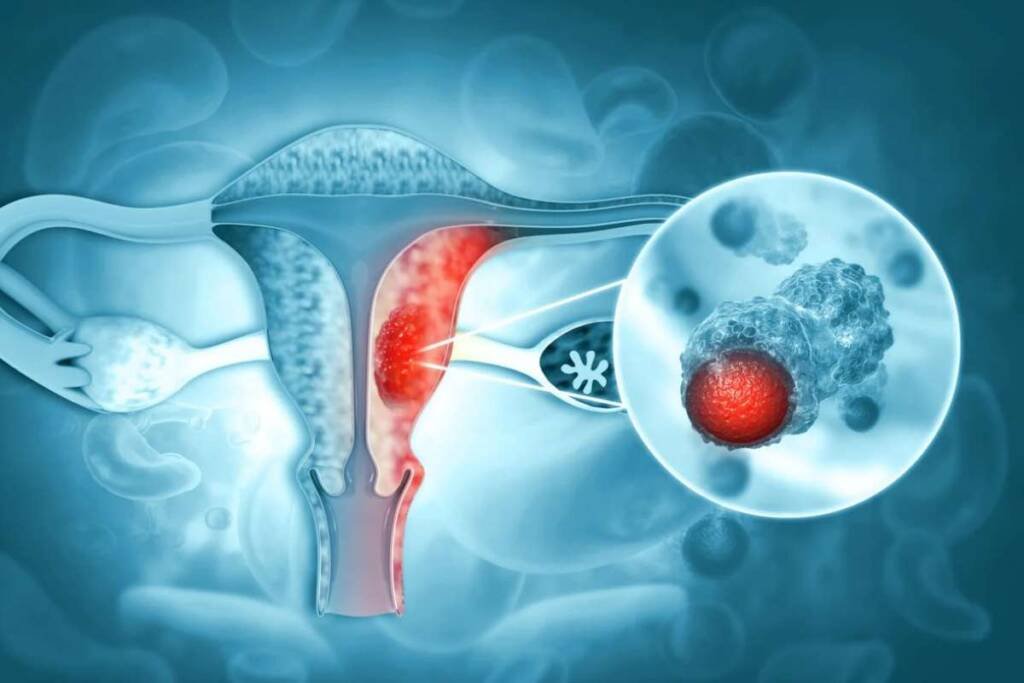
The pear-shaped organ in the female pelvis where a baby develops during pregnancy, the uterus, is affected by uterine cancer. It is the most common gynecologic cancer in the United States, with about 66,000 new cases and 13,000 deaths each year. Uterine cancer can cause abnormal vaginal bleeding, pelvic pain, and other symptoms that may affect your quality of life and fertility. However, if detected and treated early, uterine cancer can often be cured.
Quick Points to Get You Started
- Uterine cancer symptoms are noticeable body changes, while signs are measurable, like blood pressure or test results.
- There are two main types of uterine cancer: endometrial cancer and uterine sarcoma
- There are four stages of uterine cancer.
- The exact cause of uterine cancer is not known, but it is thought to be related to changes or mutations in the DNA of cells in the uterus.
What are the symptoms of uterine cancer?
Individuals diagnosed with uterine cancer may encounter a range of symptoms or indicators. Symptoms of uterine cancer denote perceivable alterations within the body, whereas signs encompass measurable changes such as blood pressure fluctuations or outcomes from laboratory tests. Collectively, the amalgamation of symptoms and signs serves to elucidate a medical condition. It is noteworthy that instances exist where individuals with uterine cancer remain devoid of the enumerated symptoms of uterine cancer. Furthermore, it is plausible for a symptom or sign to stem from a medical condition other than cancer.
- Bleeding between periods or after menopause
- Spotting or discharge that is watery or blood-tinged
- Heavier or longer periods than usual
- Painful or difficult urination
- Pelvic pain or pressure
- Pain during sex
You should schedule an appointment with your doctor right away if you have any of these signs. They may be caused by other conditions, such as fibroids or infections, but they could also be signs of uterine cancer.
Types of uterine cancer
As mentioned earlier, there are two main types of uterine cancer: endometrial cancer and uterine sarcoma. Within these types, there are different subtypes based on how the cancer cells look under a microscope. Some subtypes are more common or aggressive than others.
Some subtypes of endometrial cancer are:
- Endometrioid adenocarcinoma: This is the most common subtype and usually grows slowly and responds well to treatment.
- Serous adenocarcinoma: This is a rare and aggressive subtype that tends to spread to other organs and has a poor prognosis.
- Clear cell adenocarcinoma: This is another rare and aggressive subtype that often occurs in women with a history of exposure to diethylstilbestrol (DES), a synthetic estrogen used in the past to prevent miscarriage.
- Carcinosarcoma: This is a very rare subtype that has features of both carcinoma (cancer of epithelial cells) and sarcoma (cancer of connective tissue). It has a high risk of spreading and has a poor prognosis.
Some subtypes of uterine sarcoma are:
- Leiomyosarcoma: This is the most common subtype and originates from smooth muscle cells in the myometrium. It tends to grow fast and spread to distant sites.
- Endometrial stromal sarcoma: This is a rare subtype that originates from stromal cells in the endometrium. It usually grows slowly and spreads to nearby lymph nodes.
- Undifferentiated sarcoma: This is a very rare subtype that has no clear origin and has a poor prognosis.
Stages of uterine cancer
The stage of uterine cancer describes how far the cancer has grown and spread in the body. The stage helps determine the best treatment options and the outlook for recovery. The stage is usually determined by examining tissue samples taken during surgery or biopsy.
There are four stages of uterine cancer:
- Stage I: Only the uterus is affected by the malignancy. It may have grown into the glands or tissues of the cervix but not beyond.
- Stage II: The cancer has spread beyond the uterus to the tissues of the cervix.
- Stage III: The cancer has spread beyond the uterus and cervix to nearby organs such as the ovaries, fallopian tubes, vagina, bladder, or rectum, or to the lymph nodes in the pelvis or around the aorta (the main artery in the abdomen).
- Stage IV: The cancer has spread to distant organs such as the lungs, liver, bones, or brain, or to the lymph nodes in the groin or other parts of the body.
Causes of uterine cancer
The exact cause of uterine cancer is not known, but it is thought to be related to changes or mutations in the DNA of cells in the uterus. These mutations may be inherited from parents or acquired during a person’s lifetime. Some factors that may increase the risk of DNA damage and uterine cancer are:
- Exposure to high levels of estrogen, either from the body’s own production or from external sources such as hormone therapy or tamoxifen
- Obesity, diabetes, PCOS, and other conditions that increase insulin resistance and inflammation, which may affect hormone levels and cell growth
- Ageing, which may reduce the ability of cells to repair DNA damage and prevent abnormal cell growth
- Infection with certain viruses, such as human papillomavirus (HPV), which may interfere with cell regulation and cause cervical cancer or endometrial cancer
- Exposure to radiation or certain chemicals, such as DES, which may damage DNA and increase the risk of uterine sarcoma
What are the uterine cancer risk factors?
Anything that raises the possibility of contracting a disease is a risk factor. Having one or more risk factors does not mean that you will get uterine cancer, but it may help you and your doctor to be more alert for signs and symptoms. Likewise, having no risk factors does not mean that you will not get uterine cancer.
Some of the risk factors for uterine cancer are:
- Age: The risk of uterine cancer increases with age, especially after menopause. The diagnostic age is 62 years on average.
- Obesity: Being overweight or obese increases the risk of uterine cancer by two to four times. This is because fat tissue produces estrogen, which stimulates the growth of the endometrium.
- Hormone imbalance: Having too much estrogen and not enough progesterone in the body can cause endometrial hyperplasia, a condition in which the endometrium becomes thickened and abnormal. The possibility of acquiring endometrial cancer may rise as a result. Hormone imbalance can result from irregular ovulation, PCOS, hormone therapy, tamoxifen, or ovarian tumors.
- Family history: Having a close relative with uterine, ovarian, or colon cancer may increase the risk of uterine cancer. This may be due to inherited genetic mutations such as BRCA1, BRCA2, or Lynch syndrome.
- Reproductive history: Having no children or having them later in life may increase the risk of uterine cancer. This is because pregnancy lowers estrogen levels and protects the endometrium from overgrowth. Having more than five children may lower the risk of uterine cancer.
- Menstrual history: Having more years of menstruation may increase the risk of uterine cancer. This is because having periods before age 12 or after age 50 exposes the endometrium to more estrogen over time.
Uterine cancer diagnosis
To diagnose uterine cancer, your doctor will ask you about your medical history, symptoms, and risk factors. They will also perform a physical exam, including a pelvic exam and a Pap test. A pelvic exam is a procedure in which your doctor feels your uterus, ovaries, and other organs for any abnormalities. A Pap test is a procedure in which your doctor collects cells from your cervix and sends them to a lab for analysis.
If your doctor suspects uterine cancer, they may order some tests to confirm the diagnosis and determine the stage of the disease. These tests may include:
- Transvaginal ultrasound: This is a test that uses sound waves to create images of your uterus and other pelvic organs. A small device called a transducer is inserted into your vagina and emits sound waves that bounce off your organs and create images on a screen. This test can show how thick your endometrium is and if there are any masses or abnormalities in your uterus.
- Endometrial biopsy: This is a test that involves taking a small sample of tissue from your endometrium for microscopic examination. Your doctor may use a thin tube called a pipelle to suction out some tissue through your cervix. Or they may use a device called a hysteroscope to look inside your uterus and take tissue samples with small instruments. This test can show if there are any cancer cells in your endometrium.
- Dilation and curettage (D&C): This is a procedure that involves dilating (widening) your cervix and scraping out tissue from your uterus with a spoon-shaped instrument called a curette. Your doctor may do this if they cannot get enough tissue from an endometrial biopsy or if the results are unclear. The lab receives the tissue samples for analysis. This test can show if there are any cancer cells in your endometrium.
- Dilation and curettage (D&C): This is a procedure that involves dilating (widening) your cervix and scraping out tissue from your uterus with a spoon-shaped instrument called a curette. Your doctor may do this if they cannot get enough tissue from an endometrial biopsy or if the results are unclear. The tissue samples are also examined under a microscope for cancer cells.
If endometrial cancer is discovered, you will probably be directed to a gynecologic oncologist, a medical professional who specialises in treating cancers of the female reproductive system. Endometrial cancer staging The extent (stage) of your cancer is determined by your doctor after it has been diagnosed. Tests used to determine your cancer’s stage may include a chest X-ray, a computerized tomography (CT) scan, positron emission tomography (PET) scan and blood tests. After you have surgery to treat your cancer, the final staging of your disease may not be known. Your cancer is given a stage by your doctor using data from various tests and procedures. Roman numerals are used to denote the various stages of endometrial cancer, with I being the lowest stage and IV being the most advanced. By stage IV, the cancer has advanced to distant parts of the body or has spread to surrounding organs like the bladder.
Survival Rate of Uterine Cancer
Various categories of statistical information exist to enable medical practitioners to assess an individual’s potential for recovery from uterine cancer. These statistics fall under the umbrella of survival statistics, with a notable subset termed as the relative survival rate of uterine cancer. This metric serves as a means to anticipate the impact of a cancer diagnosis on life expectancy. The relative survival rate of uterine cancer examines the likelihood of individuals surviving a specific duration following their initial diagnosis or commencement of treatment, juxtaposed against the anticipated survival rates of comparable individuals lacking this cancer.
To illustrate this concept, consider an illustrative scenario. Please note that this example is not specific to uterine cancer. Let’s assume the 5-year relative survival rate for a particular cancer type stands at 90%. In this context, “percent” denotes the proportion out of 100. Imagine a cohort of 1,000 individuals unaffected by cancer, and based on factors like age and other attributes, it is expected that 900 of these individuals will remain alive after 5 years. Similarly, envision another group of 1,000 individuals sharing similar age and attributes to the first group, yet all afflicted by the aforementioned cancer type with a 5-year survival rate of 90%. This implies that it is projected that 810 individuals within the cancer-affected group (90% of 900) will survive after 5 years.
It is crucial to retain an understanding that survival rate statistics for individuals with uterine cancer are solely estimations. They cannot definitively predict whether an individual will experience a shortened life due to cancer or not. Instead, these statistics delineate patterns observed among cohorts of individuals previously diagnosed with the same ailment, factoring in specific disease stages.
In the United States, the 5-year relative survival rate for uterine cancer stands at 81%. This rate diverges for White and Black women, with figures of 84% and 64% respectively. Disparities arise as Black women are more prone to being diagnosed with aggressive endometrial cancers exhibiting lower survival rates. Variances in relative survival rates for uterine cancer hinge on diverse factors, encompassing cancer stage and grade, age and overall health of the individual, as well as treatment efficacy.
Upon uterine cancer diagnosis, if it remains confined to its initial site, it’s classified as “localized,” with a corresponding 5-year relative survival rate of 95%. If the cancer spreads regionally, the rate drops to 70%. In instances where the cancer has metastasized, yielding a distant spread, the rate diminishes further to 18%. Notably, approximately 44% of Black women receive diagnoses of regional, distant, or unstaged uterine cancer, in comparison to 29% of White women. “Unstaged” denotes cases where insufficient information is available to determine the disease stage. The survival rate for Black women remains lower across all stages of the disease.
Presently, the United States boasts over 600,000 survivors of uterine cancer.
Experts systematically gauge relative survival rate data for uterine cancer every 5 years. Consequently, these estimates might not encompass recent advancements in diagnostic or treatment modalities spanning the past 5 years. Should you have queries concerning this information, it is advisable to engage in a discussion with your healthcare provider. Additional insights into comprehending statistics can be pursued as well.
The statistical insights presented are drawn from the American Cancer Society’s publication “Cancer Facts & Figures 2023,” the ACS website, and the International Agency for Research on Cancer website. (Accessed in March 2023.)
Treatment Options for Uterine Cancer
The treatment options for uterine cancer depend on several factors, such as the type, stage, grade, and molecular subtype of the cancer, as well as your age, general health, and preferences. The main types of treatment for uterine cancer are:
Surgery
Surgery involves the removal of a tumor along with some surrounding healthy tissue, known as a margin, through a medical procedure. It’s usually the initial treatment for uterine cancer. A surgical specialist known as a gynecologic oncologist performs surgeries to treat gynecologic cancers. Before undergoing surgery, it’s advisable to discuss potential side effects related to the specific surgery with your healthcare team. To understand the fundamental aspects of cancer surgery, you can learn more here.
The typical surgical methods for uterine cancer are as follows:
Hysterectomy: Depending on the extent of the cancer, the surgeon performs either a simple hysterectomy (removing the uterus and cervix) or a radical hysterectomy (removing the uterus, cervix, upper part of the vagina, and nearby tissues). For postmenopausal patients, a bilateral salpingo-oophorectomy (removal of fallopian tubes and ovaries) is generally done as well.
Hysterectomy can be carried out through abdominal incision, laparoscopy, robotically (using small incisions), or vaginally. A gynecologic surgeon, specialized in female reproductive system surgeries, usually performs a hysterectomy.
Robotic-assisted surgery involves using small incisions to insert a camera and instruments. The surgeon uses robotic tools to remove the uterus, cervix, and surrounding tissue.
If the removed tissue shows no remaining cancer, additional treatment might not be required. However, regular screening is recommended to monitor for potential cancer recurrence.
Lymph Node Removal: Concurrently with a hysterectomy, the surgeon may remove lymph nodes near the tumor to assess if the cancer has spread beyond the uterus. This procedure might involve a sentinel lymph node biopsy or lymphadenectomy. The former includes injecting dye into the uterus during surgery and removing lymph nodes with dye accumulation. Sentinel node biopsy is becoming more common for uterine cancer than lymphadenectomy. The latter involves removing a group of lymph nodes.
It’s important to consult your doctor about the pros and cons of various surgical approaches and determine the most suitable one for you.
Surgical Side Effects:
Post-surgery, common short-term effects comprise pain and fatigue. Pain relief medications are prescribed as needed. Other immediate effects can encompass nausea, vomiting, difficulty with bladder emptying, and bowel movements. Initially, the diet might be limited to liquids before gradually reintroducing solid foods.
Removing ovaries leads to the cessation of sex hormone production, inducing early menopause if not already experienced. Although this reduces sex hormone levels, some hormones are still produced by adrenal glands and fat tissues. Early menopausal symptoms like hot flashes and vaginal dryness are likely. Your doctor can provide guidance on managing these symptoms.
Lymphadenectomy may cause leg swelling, known as lymphedema, which can be both short- and long-term.
After a hysterectomy, pregnancy becomes impossible. Premenopausal patients desiring future fertility should discuss options with their doctor. Sometimes, fertility preservation is feasible, involving less extensive surgery followed by hormone therapy.
Before uterine cancer surgery, addressing sexual and emotional effects is encouraged. Treatment post-surgery depends on cancer stage and grade. For grade 1 or 2 cancer that hasn’t spread deeply into the uterine wall, additional treatment might be unnecessary.
While considering post-surgery treatments, it’s essential to discuss how each treatment impacts you. Balancing treatment benefits against potential risks, including short- and long-term side effects and quality of life impact, is crucial. Your doctor can help you weigh these factors and understand their implications.
Radiation therapy
Radiation therapy involves using powerful x-rays or other particles to eliminate cancer cells. A specialist who administers radiation therapy for cancer treatment is known as a radiation oncologist. This therapy is usually carried out according to a specific schedule with a predetermined number of sessions over a defined period.
Radiation therapy can be delivered externally or internally. External-beam radiation therapy employs a machine outside the body to direct radiation towards the pelvic region or the area specified by your radiation oncologist. Alternatively, radiation can be applied internally, which is termed brachytherapy. External-beam radiation therapy may be used alone or combined with brachytherapy. In some cases, brachytherapy alone might be recommended. The more common form of radiation treatment is external-beam radiation therapy.
For certain uterine cancer patients, a combination of surgery (as discussed earlier) and radiation therapy is necessary. This radiation therapy is often administered post-surgery to eliminate any remaining cancer cells. In certain instances, radiation therapy might be given before surgery to shrink the tumor. If surgery isn’t feasible, radiation therapy could be suggested by the doctor.
Radiation therapy options for uterine cancer include treating the entire pelvis or focusing solely on the vaginal cavity, known as vaginal brachytherapy. Numerous factors influence the choice of radiation approach, but some patients with lower-risk conditions might opt for vaginal brachytherapy instead of pelvic radiation.
For specific patients, pelvic radiation could be the best choice to prevent cancer recurrence. This includes individuals with grade 3 cancer that has spread over half or more of the myometrium, those with cancer of any grade that has extended to cervix tissue, and those with cancer spreading beyond the uterus to nearby tissues or organs. Treatment post-surgery might involve radiation therapy alone, chemotherapy alone, or a combination of radiation and chemotherapy. Your doctor will guide you in choosing the appropriate treatment.
Pelvic radiation might also be considered for some individuals with grade 1 or 2 cancer that has spread over half or more of the myometrial thickness. Factors like age and cancer’s involvement in blood or lymphatic vessels play a role.
The side effects of radiation therapy depend on its extent and can encompass fatigue, skin reactions, changes in urinary frequency, and loose bowel movements. Most side effects subside shortly after treatment, but there’s a possibility of long-term effects. Discuss expectations and side effect management with your radiation oncologist.
Ongoing research aims to enhance radiation therapy by minimizing side effects and boosting effectiveness.
Chemotherapy
Chemotherapy employs medicines to eliminate cancer cells, typically by inhibiting their growth, division, and multiplication. In the case of endometrial cancer, chemotherapy is generally administered following surgery. It’s also considered if the cancer reappears after the initial treatment, known as recurrence.
A chemotherapy plan involves a specific number of cycles administered over a designated timeframe. Patients might receive one drug at a time or a combination of drugs concurrently.
The primary objectives of chemotherapy are to eradicate any remaining cancer post-surgery or to shrink the cancer and slow down its growth if it recurs or spreads to other body parts. While oral chemotherapy is an option, the majority of uterine cancer drugs are given via intravenous (IV) infusion. IV chemotherapy can be injected directly into a vein or via a catheter, a thin tube inserted into a vein.
Chemotherapy’s side effects vary based on the individual, the type and dosage of drugs, but they could include fatigue, heightened infection risk, nausea, vomiting, hair loss, reduced appetite, and diarrhea. These effects usually diminish after treatment concludes. Over the past decade, progress has been made in chemotherapy, leading to the creation of new drugs aimed at preventing and treating side effects. Examples include antiemetics to counteract nausea and vomiting and growth factors to prevent low white blood cell counts and lower infection risk.
Potential chemotherapy side effects for uterine cancer encompass future infertility (inability to conceive) and potential early menopause, particularly if a hysterectomy hasn’t been performed. It’s advisable to discuss fertility preservation with your doctor before starting treatment. In rare instances, certain drugs might cause hearing loss, while others could potentially harm the kidneys. Patients might receive extra intravenous fluids to safeguard their kidneys. Consult your doctor about the possible chemotherapy side effects you might encounter and ways to prevent or manage them.
Hormone therapy
Hormone therapy is employed to decelerate the growth of specific kinds of uterine cancer cells that carry receptors for hormones. These tumors are mainly adenocarcinomas and fall within grade 1 or 2.
For uterine cancer, hormone therapy often entails a substantial dose of the hormone progesterone, delivered in pill form. Other approaches include hormone-releasing intrauterine devices (IUDs) and aromatase inhibitors (AIs) like anastrozole (Arimidex), letrozole (Femara), and exemestane (Aromasin), which are commonly used to treat breast cancer. AIs work by reducing the amount of estrogen in the body, inhibiting its production in tissues and organs other than the ovaries. Hormone therapy might also be recommended for those who can’t undergo surgery or radiation, and it could be used alongside other treatments.
Possible hormone therapy side effects encompass fluid retention, increased appetite, sleep difficulties, muscle discomfort, and weight gain. Most of these effects are manageable with assistance from your healthcare team. It’s beneficial to discuss your expectations with your doctor.
Targeted therapy
Targeted therapy is a treatment strategy that zeroes in on the precise genes, proteins, or tissue environment contributing to the growth and survival of cancer. This approach aims to obstruct the expansion and spread of cancer cells while safeguarding healthy cells from harm.
Each tumor possesses distinct targets, and your doctor might conduct tests to pinpoint the genes, proteins, and other factors specific to your tumor. This enables doctors to align patients with the most suitable and effective treatment. Ongoing research uncovers more about particular molecular targets and fresh treatments tailored to them.
In cases of uterine cancer, targeted therapy is accessible through clinical trials and occasionally integrated into standard treatment protocols. The targeted therapy methods for uterine cancer encompass:
Anti-Angiogenesis Therapy: This approach seeks to halt angiogenesis, the process of creating new blood vessels. Since tumors require nutrients delivered by blood vessels to grow, anti-angiogenesis therapies aim to essentially “starve” the tumor. Bevacizumab (Avastin) is an anti-angiogenesis therapy utilized for treating uterine cancer.
Mammalian Target of Rapamycin (mTOR) Inhibitors: In endometrial cancer, mutations in the mTOR pathway are frequently identified. Individuals with advanced or recurring uterine cancer might receive drugs that obstruct this pathway, like everolimus (Afinitor). Ongoing research explores other drugs targeting this pathway, such as ridaforolimus and temsirolimus (Torisel), an approved targeted therapy for renal cell carcinoma, a type of kidney cancer.
Targeted Therapy for Rare Uterine Cancer: Uterine serous carcinoma, an uncommon yet aggressive subtype of endometrial cancer, is characterized by about 30% of these tumors expressing the HER2 gene. A clinical trial’s phase II demonstrated that a combination of trastuzumab (Herceptin) and chemotherapy effectively treated these tumors. Trastuzumab is a HER2-targeted therapy, predominantly utilized for HER2-positive breast cancer.
Diverse targeted therapies yield different side effects. It’s recommended to discuss these potential side effects with your doctor and explore strategies to manage them.
Immunotherapy
Immunotherapy taps into the body’s natural defenses to combat cancer. It strengthens the immune system’s ability to target and attack cancer cells.
Uterine cancers with mismatch repair defects (dMMR; as introduced earlier) are particularly responsive to immunotherapy. An immunotherapy drug called pembrolizumab (Keytruda) is authorized for treating tumors with high microsatellite instability (MSI-high) or dMMR, regardless of their location in the body. Pembrolizumab can be utilized for uterine tumors with dMMR if previous treatments have not yielded results.
Another approved approach involves combining lenvatinib (Lenvima), a targeted therapy drug, with pembrolizumab to treat advanced endometrial cancer. This combination is suitable for cases that are neither MSI-high nor dMMR, have not responded to systemic therapy, and are not treatable through surgery or radiation. Lenvatinib might cause elevated blood pressure and other side effects, necessitating vigilant monitoring and management.
In 2021, the FDA sanctioned the immunotherapy drug dostarlimab (Jemperli) to address recurring or advanced endometrial cancer with dMMR that has progressed either during or after platinum-containing chemotherapy. In 2023, the FDA expanded dostarlimab’s use to include treating individuals with recurring or advanced endometrial cancer that is dMMR or MSI-high, in combination with carboplatin and paclitaxel. Dostarlimab is administered intravenously every 3 weeks, with common side effects encompassing fatigue, nausea, diarrhea, and constipation.
Different immunotherapy forms can produce varying side effects, such as skin reactions, flu-like symptoms, diarrhea, and shifts in weight, among other potential effects. Consult your doctor to understand the potential side effects associated with the recommended immunotherapy for you.
What are the emerging uterine cancer treatment options?
Uterine cancer research is advancing rapidly, with many promising innovations on the horizon. Some of the emerging treatment options for uterine cancer are:
- Molecular profiling: This is a technique that analyses the genetic and molecular characteristics of your cancer cells, such as mutations, gene expression, or protein levels. Molecular profiling can help identify the subtype of your cancer, predict its behaviour and response to treatment, and guide the selection of the most effective and personalised therapy for you. Molecular profiling can also help detect new targets for drug development and clinical trials.
- Liquid biopsy: This is a technique that uses a blood sample to detect and monitor cancer cells or their DNA fragments (circulating tumor cells or circulating tumor DNA) in your bloodstream. Liquid biopsy can help diagnose uterine cancer, assess its stage and spread, measure its response to treatment, and detect signs of recurrence or resistance. Liquid biopsy can also help identify new targets for drug development and clinical trials.
- Artificial intelligence: This is a technique that uses computer algorithms to analyze large amounts of data and generate insights, predictions, or recommendations. Artificial intelligence can help improve the diagnosis, staging, prognosis, and treatment of uterine cancer by integrating information from various sources, such as imaging, pathology, molecular profiling, clinical records, and literature. Artificial intelligence can also help optimize the design and conduct of clinical trials and enhance patient care and outcomes.
Future directions for uterine cancer research
The future of uterine cancer research has great promise for improvements in patient outcomes, diagnosis, and treatment. Among the main areas of attention are:
- Developing new drugs and combinations that target specific molecular subtypes of uterine cancer or overcome resistance mechanisms
- Evaluating the optimal timing, sequence, and duration of multimodal therapies for different stages and subtypes of uterine cancer
- Exploring the role of immunotherapy in combination with other treatments or as maintenance therapy for uterine cancer
- Identifying biomarkers that can predict response, toxicity, or recurrence of uterine cancer
- Improving the quality of life and survivorship of patients with uterine cancer by addressing physical, psychological, social, and sexual issues
- Reducing the disparities and barriers in access to care and participation in clinical trials for patients with uterine cancer
Collaborative efforts between researchers, clinicians, patients, advocates, and industry partners are essential to driving these innovations forward.
Conclusion
Uterine cancer is a complex and heterogeneous disease that requires a multidisciplinary and personalized approach to management. The advent of molecular profiling, immunotherapy, novel drug development, liquid biopsy, and artificial intelligence are revolutionizing our understanding and treatment of uterine cancer. The goal is to achieve better outcomes for patients with uterine cancer while minimizing side effects and preserving quality of life.
FAQ’s
What are the signs and symptoms of uterine cancer?
Abnormal vaginal bleeding is uterine cancer’s most prevalent symptom. This may include bleeding between periods or after menopause, spotting or discharge that is watery or blood-tinged, heavier or longer periods than usual, painful or difficult urination, pelvic pain or pressure, or pain during sex. You should schedule an appointment with your doctor right away if you have any of these signs.
How is uterine cancer diagnosed?
To diagnose uterine cancer, your doctor will ask you about your medical history, symptoms, and risk factors. They will also perform a physical exam, including a pelvic exam and a Pap test. A pelvic exam is a procedure in which your doctor feels your uterus, ovaries, and other organs for any abnormalities.
What are the treatment options for uterine cancer?
The treatment options for uterine cancer depend on several factors, such as the type, stage, grade, and molecular subtype of the cancer, as well as your age, general health, and preferences. Surgery, radiation therapy, chemotherapy, hormone therapy, targeted therapy, and immunotherapy are the main therapeutic modalities for uterine cancer.
How can I cope with uterine cancer?
Uterine cancer can be a challenging and stressful experience that affects not only your physical health but also your emotional, social, and sexual well-being. You may face many issues such as pain, fatigue, infertility, menopause symptoms, body image changes, sexual dysfunction, relationship problems, financial difficulties, or fear of recurrence. It is normal to feel angry, sad, anxious, or depressed at times. However, you don’t have to cope alone.