ABSTRACT NUMBER – LBA9016
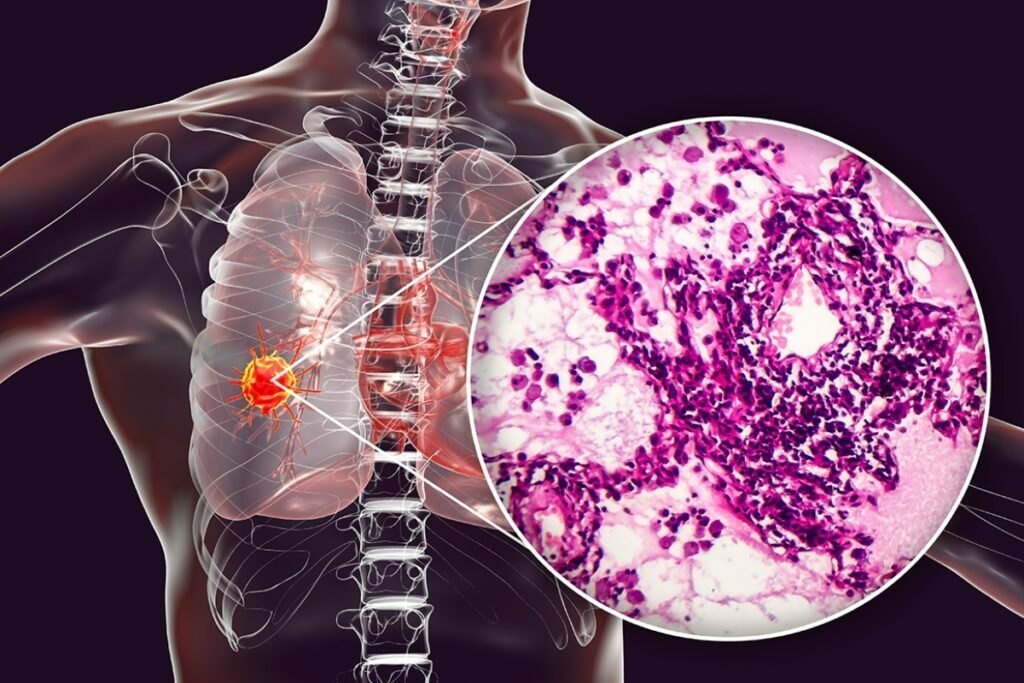
Amgen has made a courageous endeavor in cancer research over the last four decades by creating LUMAKRAS/LUMYKRAS, a specific inhibitor designed for KRASG12C. This achievement represents a significant breakthrough considering the immense challenges in targeting the KRAS G12C mutation. LUMAKRAS/LUMYKRAS has demonstrated a positive benefit-risk profile, showcasing remarkable and long-lasting anticancer activity in patients with locally advanced or metastatic non-small cell lung cancer (NSCLC) harboring the KRAS G12C mutation. This groundbreaking therapy is available as a once-daily oral formulation, providing patients convenience and ease of administration. In May 2021, the US FDA approved LUMAKRAS for treating KRAS G12C-mutated NSCLC.
Amgen’s LUMAKRAS has shown superiority over chemotherapy in preventing tumor progression in previously treated KRAS G12C-mutated NSCLC patients. Central nervous system (CNS) metastases, a regrettable common complication in advanced NSCLC with KRAS G12C mutations, affect approximately 30-40% of patients. The Phase III CodeBreaK 200 trial, the only randomized study for any KRASG12C inhibitor, included a post-hoc analysis focusing on patients with advanced NSCLC and stable CNS lesions at the beginning of the trial, as determined by an anonymous independent central review (BICR).
Through a modified exploratory response assessment called RANO-BM, this analysis revealed that LUMAKRAS exhibited a delayed time to CNS progression and a longer CNS progression-free survival (PFS) compared to the chemotherapy drug docetaxel. The post-hoc analysis of CodeBreaK 200 demonstrated that LUMAKRAS delayed CNS progression-free survival by more than five months, providing a potentially meaningful clinical benefit for second-line NSCLC patients with KRAS G12C mutations.
Moreover, the analysis showed that LUMAKRAS achieved a more than twofold increase in the CNS objective response rate (ORR), which measures the shrinkage of CNS tumors after treatment, compared to Docetaxel (33.3% vs. 15.4%). Importantly, the safety profile of LUMAKRAS in this analysis was similar to that observed in the overall population of the CodeBreaK 200 trial. Additionally, the concordance between disease control in the systemic and intracranial regions was higher with LUMAKRAS (88%) compared to Docetaxel (54%).
LUMAKRAS demonstrated improved progression-free survival (PFS) compared to Docetaxel, regardless of the level of PD-L1 expression, and maintained a PFS benefit over Docetaxel across key co-alteration subgroups, including STK11, KEAP1, and TP53. Notably, the time to CNS recurrence was 9.6 months with LUMAKRAS compared to 5.4 months with Docetaxel. These biomarker data collectively provide valuable insights for treatment decision-making and guide the ongoing development of the CodeBreaK 200 clinical trial, which explores LUMAKRAS in innovative combination therapies.
In terms of adverse events, treatment-related side effects of any grade were observed in 77.5% of patients receiving LUMAKRAS, while 89.7% of patients treated with Docetaxel experienced such events.