Everything You Need to Know About Prostate Cancer Treatment and Prevention
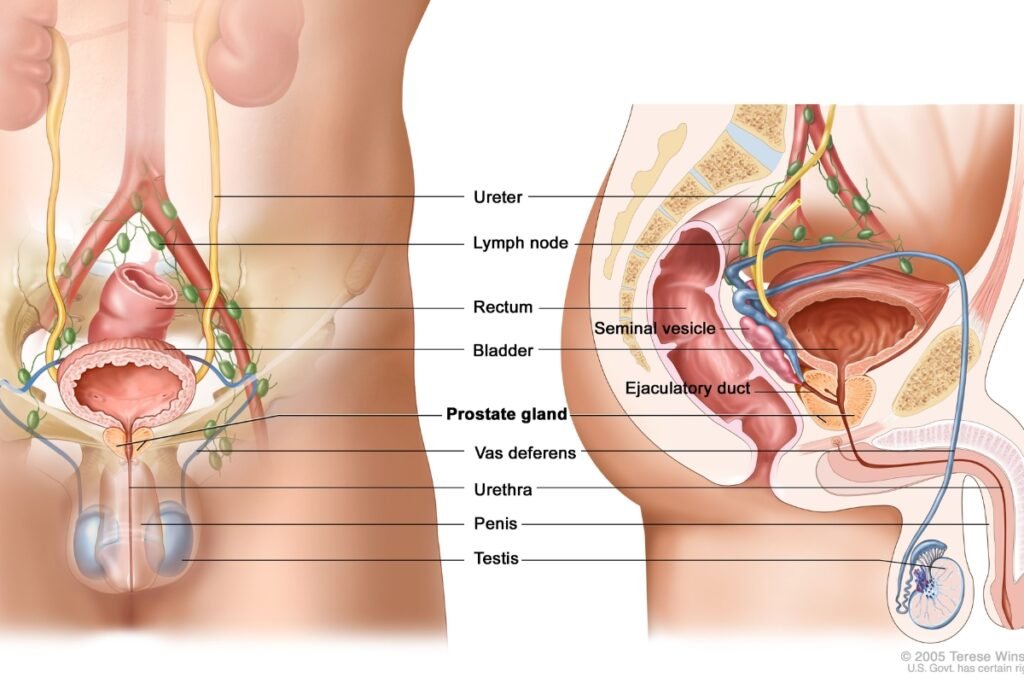
A lot of men are affected by prostate cancer, which is a kind of cancer that forms in the prostate gland. It occurs when abnormal cells grow in the prostate gland, a small organ producing fluid for semen. Prostate cancer can cause various symptoms, such as difficulty urinating, blood in urine or semen, pain in the lower back or pelvis, and erectile dysfunction. However, some men may not have any symptoms at all.
The treatment of prostate cancer depends on many factors, such as the stage and grade of cancer, the patient’s age and health, and personal preferences and goals. Different prostate cancer treatments are available, each with its benefits and risks. This blog will discuss some of the most common prostate cancer treatments and what you need to know about them.
Prostate Cancer Treatment Observation or Active Surveillance
Observation or active surveillance is an option for men with low-risk or very low-risk prostate cancer, which means the cancer is small, slow-growing, and unlikely to spread or cause problems. Observation or active surveillance involves monitoring cancer closely with regular tests, such as prostate-specific antigen (PSA), blood tests, digital rectal exams (DRE), and biopsies. Observation or active surveillance aims to avoid or delay unnecessary treatments that may cause side effects, such as impotence or incontinence. However, treatment may be recommended if the cancer shows signs of growing or spreading.
Observation or active surveillance may be suitable for men who have a life expectancy of less than 10 years, have other severe health conditions that limit their treatment options, or prefer to avoid treatments that may affect their quality of life. Observation or active surveillance requires careful follow-up and regular communication with the doctor. It also requires the patient to be comfortable with living with untreated cancer and willing to switch to active treatment if needed.
Surgery
Surgery is an option for men in prostate cancer treatment with localized or locally advanced prostate cancer, meaning that the cancer is confined to the prostate gland or has spread only to nearby tissues. Surgery involves removing the entire prostate gland and some surrounding tissues, such as the seminal vesicles and lymph nodes. This procedure is called a radical prostatectomy. There are different ways to perform radical prostatectomy, such as open, laparoscopic, or robotic-assisted surgery. The choice of surgical technique depends on the surgeon’s experience, the patient’s anatomy, and equipment availability.
The main benefit of surgery is that it can remove most or all of the cancer in prostate cancer treatment from the body and reduce the risk of recurrence or metastasis. However, surgery also has risks and side effects, such as bleeding, infection, nerve damage, urinary problems, sexual problems, and bowel problems. Some side effects may improve over time or with treatment, but some may be permanent. Surgery may also affect fertility and require artificial methods to achieve pregnancy.
Radiation Therapy in Prostate Cancer Treatment
Radiation therapy is an option for men in prostate cancer treatment with localized or locally advanced prostate cancer and for men with recurrent or metastatic prostate cancer that has spread to other body parts. Radiation therapy involves using high-energy rays or particles to kill or stop cancer cells from growing. There are two main types of radiation therapy for prostate cancer: external beam radiation therapy (EBRT) and brachytherapy.
EBRT delivers radiation from a machine outside the body to the prostate gland and nearby tissues. EBRT can be given in different ways, such as conventional radiation therapy (CRT), intensity-modulated radiation therapy (IMRT), image-guided radiation therapy (IGRT), stereotactic body radiation therapy (SBRT), or proton beam therapy (PBT). The choice of EBRT technique depends on the stage and location of the cancer, the dose and duration of radiation, and the availability of equipment.
Brachytherapy involves placing radioactive seeds or wires inside or near the prostate gland. Brachytherapy can be given in two ways: low-dose rate (LDR) or high-dose rate (HDR) brachytherapy. LDR brachytherapy involves implanting permanent radioactive seeds that release radiation slowly over several months. HDR brachytherapy involves inserting temporary radioactive wires that deliver a high dose of radiation over a short period of time.
The main benefit of radiation therapy is that it can target cancer cells while sparing most of the normal tissues around them. However, radiation therapy in prostate cancer treatment also has risks and side effects, such as skin irritation, fatigue, urinary problems, sexual problems, bowel problems, and bladder or rectal cancer. Some side effects may improve over time or with treatment, but some may be permanent. Radiation therapy may also affect fertility and require artificial methods to achieve pregnancy.
Hormone Therapy
Hormone therapy is an option for men with advanced or metastatic prostate cancer in prostate cancer treatment that has spread to other body parts. Hormone therapy involves using drugs or surgery to lower the levels of male hormones, such as testosterone, that stimulate the growth of prostate cancer cells. Different types of hormone therapy for prostate cancer, such as androgen deprivation therapy (ADT), anti-androgens, or newer hormonal agents.
ADT involves using drugs that stop testosterone production by the testicles or block its action on the prostate cancer cells. ADT can be given in different ways, such as injections, implants, pills, or patches. ADT can be given continuously or intermittently, depending on the stage and progression of the cancer.
Anti-androgens are drugs that block the action of testosterone on prostate cancer cells. Anti-androgens can be used alone or in combination with ADT to prevent or delay the development of resistance to ADT.
Newer hormonal agents target specific pathways or mechanisms that allow prostate cancer cells to grow and survive despite low testosterone levels. Newer hormonal agents can be used alone or in combination with ADT or chemotherapy to treat advanced or metastatic prostate cancer that has become resistant to other treatments.
The main benefit of hormone therapy in prostate cancer treatment is that it can shrink the tumor, slow its growth, relieve symptoms, and improve survival. However, hormone therapy also has risks and side effects, such as hot flashes, weight gain, muscle mass and strength loss, osteoporosis, diabetes, heart disease, mood changes, memory problems, and sexual problems. Some side effects may improve over time or with treatment, but some may be permanent. Hormone therapy also affects fertility and requires artificial methods to achieve pregnancy.
Chemotherapy
Chemotherapy is an option for men with advanced or metastatic prostate cancer that has spread to other parts of the body and has become resistant to hormone therapy. Chemotherapy involves using drugs that kill cancer cells or stop them from dividing. Chemotherapy can be given in different ways, such as intravenous (IV) infusion, oral pills, or injections. Chemotherapy can be given alone or in combination with hormone therapy or newer hormonal agents.
The main benefit of chemotherapy in prostate cancer treatment is that it can shrink the tumor, slow its growth, relieve symptoms, and improve survival. However, chemotherapy also has risks and side effects, such as hair loss, nausea, vomiting, diarrhea or constipation, mouth sores, loss of appetite and weight, infection, bleeding or bruising easily, fatigue, and anemia. Some side effects may improve over time or with treatment, but some may be permanent. Chemotherapy also affects fertility and requires artificial methods to achieve pregnancy.
Immunotherapy
Immunotherapy is an option for men with advanced or metastatic prostate cancer that has spread to other parts of the body and has become resistant to hormone therapy or chemotherapy. Immunotherapy involves using substances stimulating the body’s immune system to fight cancer cells. There are different types of immunotherapy for prostate cancer, such as vaccines or checkpoint inhibitors.
Vaccines are substances that expose the immune system to antigens (proteins) that are specific to prostate cancer cells. This triggers an immune response that targets and destroys the cancer cells. Vaccines can be made from the patient’s own cells (autologous) or someone else’s cells (allogeneic).
One vaccine that is approved for prostate cancer is sipuleucel-T (Provenge). This vaccine is made specifically for each man. To make it, white blood cells (immune system cells) are removed from your blood over a few hours while you are hooked up to a special machine. The cells are then sent to a lab and mixed with a protein from prostate cancer cells called prostatic acid phosphatase (PAP). The white blood cells are then sent back to the doctor’s office or hospital, where they are given back to you by infusion into a vein (IV). This process is repeated 2 more times, 2 weeks apart, to get 3 doses of cells. The cells help your other immune system cells attack prostate cancer.
The vaccine is used for prostate cancer treatment that’s no longer responding to hormone therapy but is causing few or no symptoms. The vaccine hasn’t been shown to stop prostate cancer from growing, but it seems to help men live several months longer.
Common side effects from the vaccine can include fever, chills, fatigue, back and joint pain, nausea, and headache. These most often start during the cell infusions and last no more than a couple of days. A few men may have more severe symptoms, such as breathing problems and high blood pressure, which usually improve after treatment.
Checkpoint inhibitors block proteins on the surface of immune cells (T cells) that normally prevent them from attacking normal cells. This allows the T cells to recognize and attack the cancer cells more effectively.
Some checkpoint inhibitors that are approved for prostate cancer are:
- Pembrolizumab (Keytruda) can be used for people whose prostate cancer cells have tested positive for specific gene changes, such as a high level of microsatellite instability (MSI-H) or changes in one of the mismatch repair (MMR) genes. Changes in MSI or in MMR genes (or both) are often seen in people with Lynch syndrome. The drug is used for people whose cancer starts growing again after chemotherapy.
- Nivolumab (Opdivo) can be used with another drug called ipilimumab (Yervoy) for people whose prostate cancer has grown after hormone therapy and chemotherapy.
Common side effects of checkpoint inhibitors can include skin irritation, rash, itching, fatigue, diarrhea, nausea, loss of appetite, and inflammation of organs (such as lungs, liver, and kidneys).
Conclusion
Prostate cancer is a complex and diverse disease that requires personalized and multidisciplinary treatment. Many options are available for prostate cancer treatment, each with its advantages and disadvantages. Treatment choice depends on the stage and grade of cancer, the patient’s age and health, and personal preferences and goals.
Immunotherapy is a newer treatment that can help some men with advanced or metastatic prostate cancer that has become resistant to other treatments. Immunotherapy stimulates the body’s immune system to fight cancer cells. However, immunotherapy is ineffective for everyone and may cause some side effects.
Talk to your doctor about the best treatment options if you have prostate cancer. Consider joining a clinical trial, a research study that tests new drugs or treatment methods. Clinical trials can offer access to new and promising treatments that are not yet widely available. You can learn more about clinical trials for prostate cancer here.
Remember that you are not alone in your journey with prostate cancer. Many resources and support groups are available to help you cope with the physical, emotional, and practical challenges of living with prostate cancer. You can find some of these resources here.
We hope this blog has been informative and helpful to you. If you have any questions or comments, please leave them below. Thank you for reading!
FAQ’s
Q: What is prostate cancer, and how is it diagnosed?
A: Prostate cancer is a type of cancer that affects the prostate gland, which is part of the male reproductive system. Prostate cancer can cause symptoms such as difficulty urinating, blood in the urine, erectile dysfunction, and pain in the pelvis or back. A physical exam, blood tests, imaging tests, and prostate tissue biopsy diagnose prostate cancer.
Q: What are the main types of prostate cancer treatment, and how do they work?
A: The main types of prostate cancer treatment are surgery, radiation therapy, hormone therapy, chemotherapy, immunotherapy, and targeted therapy. Surgery involves removing the prostate gland and some surrounding tissue. Radiation therapy uses high-energy rays or particles to kill cancer cells or shrink tumors. Hormone therapy blocks or lowers the levels of male hormones that stimulate prostate cancer growth. Chemotherapy uses drugs to kill cancer cells or stop them from dividing. Immunotherapy boosts the body’s natural defenses to fight cancer. Targeted therapy uses drugs that target specific genes or proteins involved in prostate cancer growth or survival.
Q: What are the benefits and risks of each type of prostate cancer treatment?
A: The benefits and risks of each type of prostate cancer treatment depend on various factors, such as the stage and grade of cancer, the patient’s age, and overall health, the patient’s preferences and goals, and the potential side effects. Some general benefits and risks are:
- Surgery can offer a chance of curing localized or early-stage prostate cancer, but it can also cause complications such as bleeding, infection, urinary incontinence, erectile dysfunction, and damage to nearby organs.
- Radiation therapy can shrink tumors and relieve symptoms, but it can also damage healthy tissue and cause side effects such as skin irritation, fatigue, urinary problems, bowel problems, erectile dysfunction, and increased risk of secondary cancers.
- Hormone therapy can slow down or stop the growth of prostate cancer, but it can also cause side effects such as hot flashes, weight gain, loss of muscle mass, osteoporosis, mood changes, sexual problems, and increased risk of heart disease and diabetes.
- Chemotherapy can kill or slow down the growth of advanced or metastatic prostate cancer, but it can also cause side effects such as nausea, vomiting, hair loss, mouth sores, low blood cell counts, increased risk of infection and bleeding, kidney damage, nerve damage, and hearing loss.
- Immunotherapy can stimulate the immune system to attack cancer cells, but it can also cause side effects such as flu-like symptoms, rash, itching, fatigue, fever, chills, nausea, diarrhea, low blood pressure, and allergic reactions.
- Targeted therapy can block specific pathways that drive prostate cancer growth or survival, but it can also cause side effects such as fatigue, nausea, diarrhea, rash, liver damage, high blood pressure, bleeding, and blood clots.
Q: How do I choose the best prostate cancer treatment for me?
A: The best prostate cancer treatment for you depends on your individual situation and preferences. You should discuss your diagnosis, prognosis, treatment options, benefits, risks, side effects, costs, and quality of life with your doctor. You should also consider getting a second opinion from another specialist or joining a clinical trial that tests new or experimental treatments. You should weigh the pros and cons of each option and make an informed decision that suits your goals and values.
Q: What are some tips for coping with prostate cancer treatment and its side effects?
A: Some tips for coping with prostate cancer treatment and its side effects are:
- Follow your doctor’s instructions on how to prepare for and recover from your treatment.
- Ask your doctor about ways to prevent or manage your side effects, such as medications, supplements, lifestyle changes, or complementary therapies.
- Seek support from your family, friends, health care team, counselor, support group, or online community.
- Stay physically active, eat a balanced diet, drink plenty of water, get enough rest, and avoid smoking and alcohol.
- Express your feelings, concerns, fears, hopes, and goals to someone you trust or write them down in a journal.
- Find activities that make you happy, relaxed, or fulfilled, such as hobbies, music, meditation, reading, or spirituality.