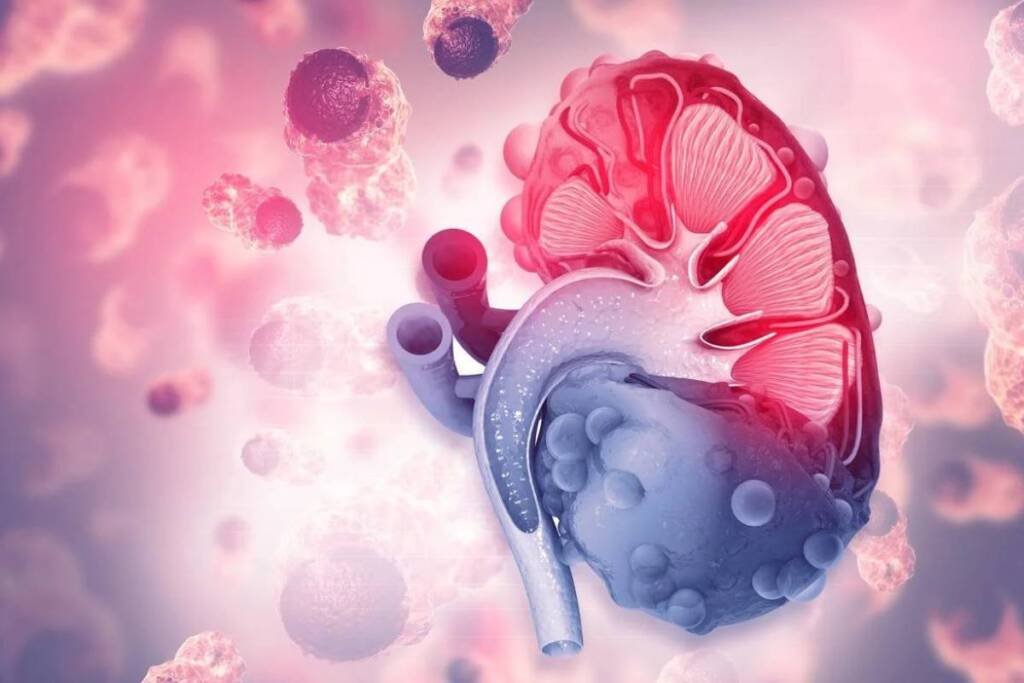
Immunotherapy has revolutionized the treatment of metastatic renal cell carcinoma (RCC), a type of kidney cancer that is often resistant to conventional therapies. One of the most effective immunotherapy combinations for metastatic RCC is nivolumab and cabozantinib, which target the PD-1 and VEGF pathways, respectively. In a clinical trial called CheckMate 9ER, this combination improved overall survival, progression-free survival, and objective response rate compared with sunitinib, a standard VEGF inhibitor.
However, immunotherapy is not without challenges. One of the main questions that patients and physicians face is how long to continue immunotherapy and what to do after stopping it. In this blog, we will discuss some of the key issues and data regarding immunotherapy discontinuation in metastatic RCC.
When to stop immunotherapy?
According to the trial design of CheckMate 9ER, patients received nivolumab and cabozantinib until disease progression or unacceptable toxicity. However, nivolumab was stopped after 2 years of treatment, while cabozantinib was continued as maintenance therapy. This is based on the general principle that immunotherapy does not provide any additional benefit after 2 years of treatment, regardless of the type of cancer. This principle is supported by data from other trials that showed no difference in outcomes between patients who continued or stopped immunotherapy after 2 years.
However, not all patients are comfortable with stopping immunotherapy after 2 years. Some patients may feel anxious or reluctant to stop a treatment that has been working for them. Therefore, it is important to educate patients early on about the rationale and expectations of immunotherapy discontinuation. Patients should be reassured that stopping immunotherapy does not mean that they will lose their response or have an immediate relapse. In fact, data from CheckMate 9ER showed that patients who stopped nivolumab after 2 years had a median time to subsequent therapy of 20.6 months, meaning that they remained stable for almost 2 years without any treatment.
What to do after stopping immunotherapy?
Another question that patients and physicians face is what to do after stopping immunotherapy. In CheckMate 9ER, most patients who progressed on nivolumab and cabozantinib received another TKI as second-line treatment, mainly cabozantinib. This suggests that TKIs are still effective after immunotherapy failure. However, the efficacy of TKIs may depend on the molecular subtype and the first-line treatment of the tumor.
The BIONIKK trial was a phase 2 trial that enrolled patients with metastatic RCC who had different molecular subtypes and biomarkers, and randomized them to receive either nivolumab alone, nivolumab and ipilimumab (another immunotherapy combination), or a TKI in the frontline setting. The trial showed that some subtypes responded better than others to different treatments. For example, patients with ccRCC-4 subtype, which is characterized by high immune gene expression and low angiogenesis gene expression, had better outcomes with nivolumab and ipilimumab than with nivolumab alone or TKI. On the other hand, patients with ccRCC-2 subtype, which is characterized by low immune gene expression and high angiogenesis gene expression, had similar outcomes with nivolumab and ipilimumab or TKI.
The BIONIKK trial also showed that the choice of first-line treatment influenced the outcomes of second-line treatment after progression. Most patients who progressed on any first-line treatment received a TKI as second-line treatment, mainly cabozantinib. However, the efficacy of TKI as second-line treatment seemed to be higher in patients who received nivolumab and ipilimumab as first-line treatment than in those who received nivolumab alone or TKI as first-line treatment. For example, patients with ccRCC-4 subtype who received nivolumab and ipilimumab as first-line treatment had a 33% response rate and a median progression-free survival of 12 months with TKI as second-line treatment, compared with 11% response rate and 8 months progression-free survival in those who received nivolumab alone or TKI as first-line treatment.
These results suggest that nivolumab and ipilimumab may have a long-lasting effect on the tumor microenvironment and the immune system, making the tumor more sensitive to subsequent TKI treatment. Alternatively, TKI may have a negative impact on the immune system, making the tumor more resistant to subsequent nivolumab and ipilimumab treatment. These hypotheses need to be further investigated in future studies.
How to manage toxicity?
One of the main concerns of immunotherapy is toxicity. Immunotherapy can cause immune-related adverse events, such as inflammation of various organs, that may require treatment interruption or discontinuation. These events can be managed with steroids or other immunosuppressive drugs, but they can also affect the quality of life of patients. Therefore, it is important to monitor patients closely and educate them about the signs and symptoms of potential complications.
The CheckMate 9ER trial showed that nivolumab and cabozantinib had a manageable safety profile compared with sunitinib. The rate of treatment discontinuation due to adverse events was similar between nivolumab and cabozantinib (27.2%) and sunitinib (10.3%). However, the rate of dose reduction was higher with nivolumab and cabozantinib (51.5%) than with sunitinib (36.8%). The most common adverse events with nivolumab and cabozantinib were diarrhea, fatigue, hypertension, and rash.
The BIONIKK trial showed that nivolumab and ipilimumab had a higher rate of treatment discontinuation due to adverse events (22%) than nivolumab alone (12%) or TKI (10%). The most common adverse events with nivolumab and ipilimumab were diarrhea, fatigue, rash, and hypothyroidism.
Conclusion
Immunotherapy discontinuation in metastatic RCC is a complex and individualized decision that requires careful counseling and shared decision-making between patients and physicians. Patients should be informed about the benefits and risks of stopping or continuing immunotherapy, as well as the options and expectations for subsequent treatment. Physicians should also consider the molecular subtype and biomarker status of the tumor, as well as the toxicity profile and patient preference, when choosing the best treatment strategy for each patient. Immunotherapy has opened new horizons for metastatic RCC, but more research is needed to optimize its use and maximize its potential.