Imagine a world where you could treat cancer with a simple injection or infusion, without the need for surgery, chemotherapy, or radiation. Sounds too good to be true, right?
Well, that’s the vision behind BCMA-targeted therapies, a new class of drugs that aim to wipe out multiple myeloma, a type of blood cancer that affects plasma cells.
BCMA stands for B cell maturation antigen, and it’s a protein that’s found on the surface of plasma cells and some B cells. It helps these cells survive and grow, which is good for normal immune function, but bad for multiple myeloma.
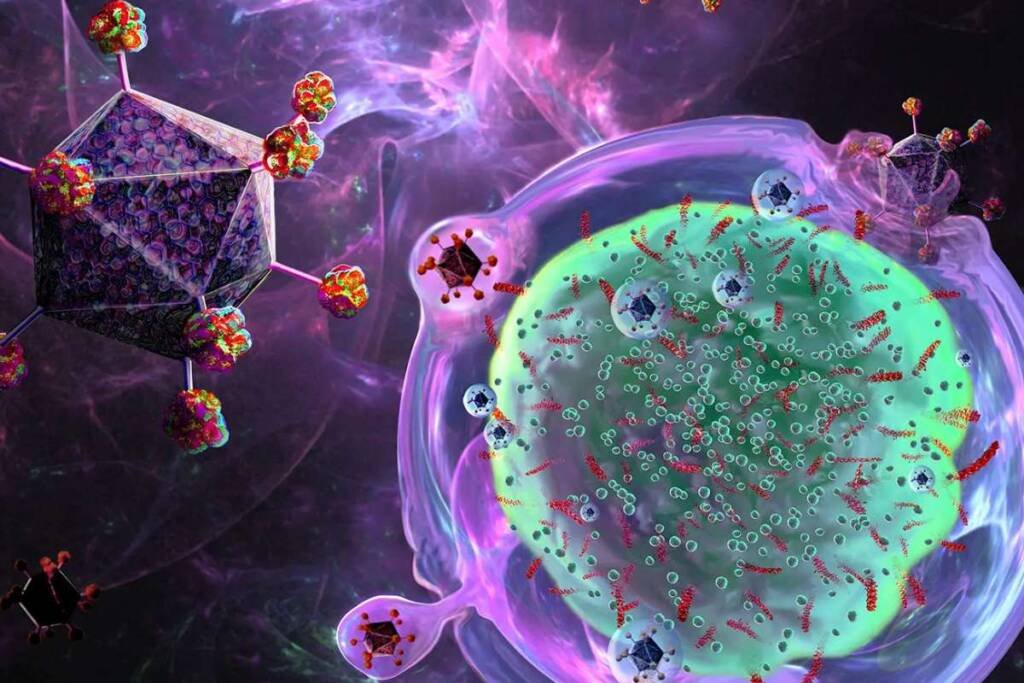
That’s why researchers have been developing therapies that target BCMA and kill the cancerous plasma cells, while sparing the healthy ones. These therapies include:
- Monoclonal antibodies, which are proteins that bind to BCMA and flag the plasma cells for destruction by the immune system.
- Antibody-drug conjugates, which are monoclonal antibodies that carry a toxic payload that is released when they bind to BCMA and enter the plasma cells.
- CAR T-cell therapy, which involves collecting and modifying the patient’s own immune cells (called T cells) to make them recognize and attack BCMA.
- Radioligand therapy, which involves injecting a radioactive substance that binds to BCMA and delivers radiation to the plasma cells.
These therapies have shown remarkable results in clinical trials, shrinking tumors and extending survival in patients with multiple myeloma who have exhausted other options. Some patients have even achieved complete remission, meaning no signs of cancer in their blood or bone marrow.
But before you get too excited, there’s a catch. BCMA-targeted therapies are not perfect. They come with their own challenges and limitations, such as:
- Safety issues. Some of these therapies can cause serious side effects, such as infusion reactions, low blood counts, infections, nerve damage, or cytokine release syndrome (CRS), a potentially life-threatening inflammatory reaction that can occur with CAR T-cell therapy.
- Efficacy issues. Some of these therapies may not work for everyone, or may stop working over time. Some patients may develop resistance to BCMA-targeted therapies, or lose BCMA expression on their plasma cells.
- Accessibility issues. Some of these therapies are not widely available or affordable. Some of them require complex procedures, such as collecting and modifying the patient’s own immune cells (for CAR T-cell therapy), or injecting radioactive substances into the bloodstream (for radioligand therapy). Some of them may not be covered by insurance or reimbursed by health systems.
So how do physicians feel about these new options for multiple myeloma? A recent survey conducted by Targeted Oncology asked 100 hematologists-oncologists about their perceptions and preferences of BCMA-targeted therapies.
The results were mixed. On one hand, most physicians agreed that BCMA is a promising target and that these therapies have shown impressive results in clinical trials. On the other hand, they also expressed concerns about the safety, efficacy, and accessibility of these treatments.
For example, 72% of physicians said they were worried about the risk of CRS with CAR T-cell therapy. 68% said they were unsure about the durability of response with BCMA-targeted therapies. And 64% said they were concerned about the availability and cost of these treatments, especially for patients who live in rural areas or have limited insurance coverage.
The survey also revealed some differences in preferences among physicians. For instance, 44% said they would prefer to use an antibody-drug conjugate as a first-line BCMA-targeted therapy, while 32% said they would choose a monoclonal antibody. Only 12% said they would opt for CAR T-cell therapy, and 8% for radioligand therapy.
Of course, these preferences may change as more data and experience become available. The survey also showed that physicians were eager to learn more about BCMA-targeted therapies and how to best use them in clinical practice.
As of 2023, there are four BCMA-targeted therapies approved by the FDA for multiple myeloma. The first one, approved in 2020, was belantamab mafodotin (Blenrep), an antibody-drug conjugate developed by GlaxoSmithKline. The second one, approved in 2021, was idecabtagene vicleucel (Abecma), a CAR T-cell therapy developed by Bristol Myers Squibb. The third one, approved in 2022, was teclistamab (Tecartus), a bispecific antibody developed by Janssen. The fourth one, approved in 2022, was ciltacabtagene autoleucel (Carvykti), another CAR T-cell therapy developed by Janssen and Legend Biotech . These therapies offer different advantages and disadvantages in terms of safety, efficacy, and accessibility, and may be suitable for different subsets of patients with multiple myeloma.
So what does this mean for you, dear reader? If you have multiple myeloma or know someone who does, you may want to keep an eye on BCMA-targeted therapies. They could be the next big thing in cancer treatment, or at least a valuable addition to the existing arsenal.
But don’t get too excited yet. These therapies are still experimental and not widely available. They may also come with some drawbacks and uncertainties that need to be weighed carefully against their benefits.
The bottom line is: talk to your doctor. Ask them about BCMA-targeted therapies and whether they are suitable for your situation. And remember: you are not alone in this journey. There are many resources and support groups that can help you cope with multiple myeloma and its treatment.
Thank you for reading this article. If you found it informative and entertaining, please share it with your friends and family. And don’t forget to subscribe to our newsletter for more updates on BCMA-targeted therapies and other topics related to cancer care.