The landscape of HIV therapies has evolved significantly since the 1980s, when the FDA first approved the pioneering antiretroviral therapy AZT. Patients have transitioned from consuming multiple daily pills to just two or fewer, thanks to the advent of long-acting injectable drugs that require administration only once a month. In a groundbreaking development, a team of biomedical engineers at Johns Hopkins University School of Medicine has introduced an innovative injectable hydrogel. This hydrogel, as reported in the Journal of the American Chemical Society on September 25, sustains plasma concentrations of the common HIV drug lamivudine (also known as 3TC) for an impressive six weeks in mice. The researchers envision expanding this hydrogel platform to accommodate multiple HIV drugs simultaneously, streamlining treatment.
“This is a novel way to deliver anti-HIV meds, and this platform has the advantage that a single polymer can be programmed to deliver several different drugs simultaneously.”
– co-author Charles Flexner, M.D
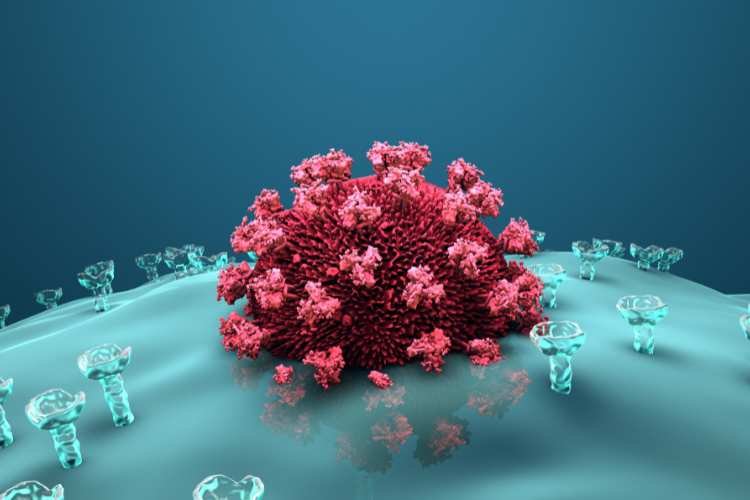
Unlike conventional delivery systems or carriers, this hydrogel represents a unique formulation of the drug itself. Injected beneath the skin, it self-assembles into a reservoir-like structure that gradually releases its contents into the bloodstream. After fine-tuning the polymer to enhance its durability, the researchers administered it to five adult male mice, comparing its performance to a control group receiving 3TC injections without the hydrogel.
Also Read: Some Individuals’ Cognitive Deterioration May Be Slowed By Hearing Aids
In the control group, drug levels became undetectable by Day 3, whereas in the experimental group, concentrations continued to rise until Day 7. Subsequently, they remained at levels sufficient to suppress HIV for an additional 36 days. Remarkably, even on Day 49, the drug remained at high concentrations in vital tissues like the liver, spleen, lymph nodes, lungs, and kidneys.
The researchers are actively exploring ways to incorporate other commonly used HIV drugs alongside 3TC within the hydrogel. Furthermore, they anticipate extending dosing intervals to “several months or even longer” by optimizing the hydrogel’s design and drug dosage, potentially positioning it as an HIV prophylaxis.
“Keeping the high drug levels in plasma for 42 days is very impressive. But in the future, we hope it will be even longer.” The primary challenge in HIV treatment is the need for lifelong management of the virus. This new molecular design shows us a future in which drug hydrogelation can do that to improve HIV treatment.”
– Honggang Cui, Ph.D, lead researcher
Additionally, the researchers highlighted the hydrogel’s potential effectiveness against hepatitis B since lamivudine is used to treat this virus as well. Given the frequent co-occurrence of hepatitis B with HIV, this hydrogel presents an advantage over existing injectable HIV therapies, which exclusively target the HIV virus. Notably, the hydrogel can already be adapted to accommodate tenofovir, a standard-of-care therapy for chronic hepatitis B and another vital component in the HIV treatment and prevention arsenal.